Day: August 10, 2009
Health care reform and primary sources
One thing I always encourage my residents and students to do is to go to primary sources. If someone tells you that thiazide diruetics should be the first line treatment for hypertension, get on MedLine and see if that assertion is congruent with the evidence. It’s important to see how we arrive at broad treatment recommendations, how strong and consistent the evidence...
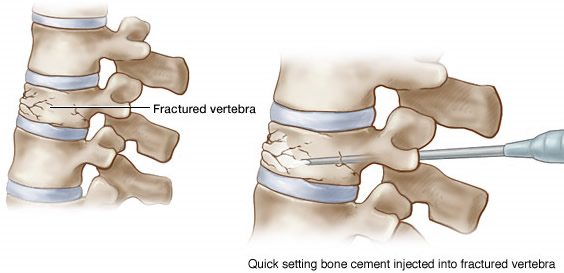
Vertebroplasty for compression fractures due to osteoporosis: Placebo medicine
When seemingly science-based medicine turns out to be placebo medicine.

