Month: May 2010
Welcoming a new blogger to SBM
It is my pleasure to announce the addition of a new SBM blogger. Impressed by his dedication to applying scientific principles to the profession of pharmacy, we have recruited Scott Gavura, who is currently best known for his work on Science-Based Pharmacy. You can find out a bit more about his background at his new page on SBM, and his first post...
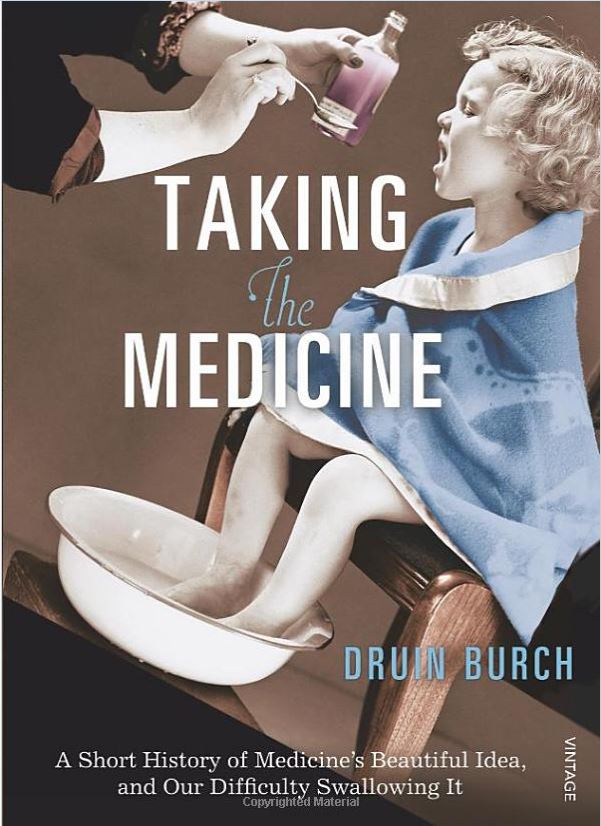
Medicine’s Beautiful Idea
For most of human history, doctors have killed their patients more often than they have saved them. An excellent new book, Taking the Medicine: A Short History of Medicine’s Beautiful Idea, and Our Difficulty Swallowing It, by Druin Burch, MD, describes medicine’s bleak past, how better ways of thinking led to modern successes, and how failure to adopt those better ways of...
The 2008-2009 Report of the President’s Cancer Panel: Mostly good, some bad, and a little ugly
Mark Crislip is always a hard act to follow, particularly when he’s firing on all cylinders, as he was last Friday. Although I can sometimes match him (and, on rare occasions, even surpass him) for amusing snark, this time around I’m going to remain mostly serious because that’s what the subject matter requires. I’ve said it before and I’ll say it again:...
Nine Questions, Nine Answers.
This is not an easy blog to write. Doctors Novella and Gorski want the entries to be formal, academic, referenced, with a minimum of snark. For the most part I comply. But sometimes. Sometimes. It is hard, so hard, not to spiral into sarcastic diatribes over the writings that pass for information on the interwebs. How should one respond to profound ignorance...
How do religious-based hospitals affect physician behavior?
Science-based medicine is, among other things, a tool. Science helps us sequester our biases so that we may better understand reality. Of course, there is no way to avoid being human; our biases and our intuition still betray us, and when they do, we use other tools. Ethics help us think through situations using an explicitly-stated set of values that most of...
Low Dose Naltrexone – Bogus or Cutting Edge Science?
On SBM we have documented the many and various ways that science is abused in the pursuit of health (or making money from those who are pursuing health). One such method is to take a new, but reasonable, scientific hypothesis and run with it, long past the current state of the evidence. We see this with the many bogus stem cell therapy...
Food Allergies and Food Addiction
Last week I wrote about the CME presentations at an obesity course put on by the American Society of Bariatric Physicians. I saved the most controversial one for last. Dr. Kendall Gerdes is a former president of the American Academy of Environmental Medicine, which I have previously written about. The AAEM is not recognized by the American Board of Medical Specialties and...
Pediatric Chiropractic Care: Scientifically Indefensible?
In a paper published in 2008, two academic chiropractors offered this observation: “The health claims made by chiropractors with respect to the application of manipulation as a health care intervention for pediatric health conditions continue to be supported by only low levels of scientific evidence. Chiropractors continue to treat a wide variety of pediatric health conditions.”1 Despite lack of support by the...

