In the age of the COVID-19 pandemic, can we trust the CDC and FDA any more?
Since the COVID-19 pandemic reached the US, increasing concern has been expressed about the politicization of the CDC and FDA due to pressure from the Trump administration to downplay the severity of the pandemic and push out treatments and a vaccine as fast as possible, potentially at the expense of safety. This has led me to a disturbing question: Can I trust...

Don’t use a COVID-19 vaccine, cry the antivaxxers, because of the horseshoe crab!
Antivaxxers are now urging vegans not to use a COVID-19 vaccine because blood from horseshoe crabs will be used in its manufacture. At its heart, this is no different than their weaponization of beliefs against other vaccine ingredients, except that it does use a germ of a good point that we should be looking for other ways to ensure that vaccines have...

Does convalescent plasma work against COVID-19? Who knows?
Last night, the FDA issued an emergency use authorization (EUA) for convalescent plasma to treat COVID-19, even though there are no randomized clinical trials demonstrating efficacy and safety. Does this plasma work? Who knows? But that didn't stop the FDA from issuing the EUA, almost certainly as a result of intense political pressure from the Trump Administration.

Announcement: The Society for Science-Based Medicine is becoming part of the Center for Inquiry
The Society for Science-Based Medicine is no more. Long live the Society for Science-Based Medicine as part of the Center for Inquiry.

HCQTrial.com: Astroturf and disinformation about hydroxychloroquine and COVID-19 on steroids
Late last week, a "study" published on HCQTrial.com by an anonymous source claiming to be a group of PhD scientists went viral. It claimed that countries that used hydroxychloroquine to treat COVID-19 had a 79% lower fatality rate than those who didn't. It was horrible science and quickly debunked on Twitter by several epidemiologists. That didn't stop it from going viral. Disinformation...

The perils and pitfalls of “doing your own research” about COVID-19 (or any other science)
Ethan Siegel at Forbes argues that you "must not 'do your own research.'" While the title grates, Siegel is correct that most of us are not really capable of "doing our own research" about most scientific and medical questions because we lack the necessary background. We must therefore be humble and be very, very careful about "doing our own research."
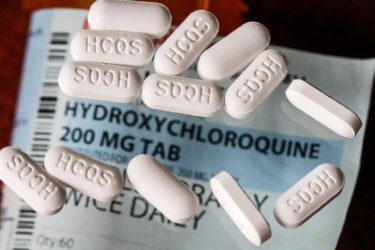
Hydroxychloroquine to treat COVID-19: Evidence can’t seem to kill it
Despite the accumulating negative evidence showing that hydroxychloroquine doesn't work against COVID-19, activists continue to promote it as a way out of the pandemic. This week, the AAPS and a Yale epidemiologist joined the fray with embarrassingly bad arguments.
COVID-19 “super-spreaders” and “super-spreading events”: The controversy
Evidence is emerging suggesting that COVID-19 does not spread equally. A minority of infected individuals seem to spread the virus easily to many people, while most infected individuals spread it to few others or no one at all, likely through a combination of circumstance, environment, and possibly biology. Why is this, and what does it mean for coronavirus containment strategies?
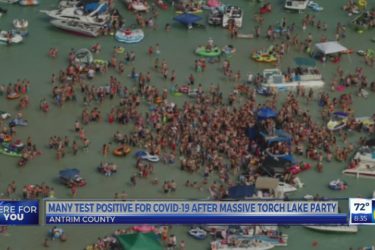
COVID-19 parties: Urban legend or real thing?
You've probably seen breathlessly scolding stories in the media about young people holding "COVID parties", in which attendees intentionally try to become infected with COVID-19. Are these parties really a thing, or are they an urban legend? The answer is not entirely clear yet, but current evidence (more specifically, the lack of evidence) for them is much more consistent with the latter...


