
Is the ACCME cracking down on quackery in continuing medical education (CME) offerings? Richard Jaffe thinks so.
Richard Jaffe, a lawyer who has made a career out of defending quacks like Dr. Stanislaw Burzynski, thinks that the ACCME, the main accrediting body for continuing medical education (CME) credits, is cracking down on "complementary and alternative medicine" CME courses. That would be a very good thing indeed, but is it really happening? More importantly, would it be enough?

“Chemotherapy is for losers”: A tragic tale of cancer, naturopathic quackery, and murder
When a patient and her family trust a naturopath rather than oncologists and oncologic surgeons, the result is often tragic. In this case, Fikreta Ibrisevic trusted naturopath Juan Sanchez Gonzalez instead of real doctors to treat her rhabdomyosarcoma in 2015. The results were as tragic as expected, and she died. What happened next was not expected and amplified the horror of the...

The Texas Medical Board lets Stanislaw Burzynski off lightly: A cautionary tale of the failure of regulating medicine
After three years and countless twists and turns, the final decision by the Texas Medical Board on the sanctions to be imposed on Houston cancer quack Dr. Stanislaw Burzynski were announced on Friday. Sadly, they were not enough. The Burzynski saga should serve as a cautionary tale that the regulation of physicians and medicine is too lax, not too strict.

Google delists Mike Adams’ Natural News website. Was it because of fake news?
Last week, in a surprise move Google delisted Mike Adams' Natural News website. Predictably, Adams immediately cried "Conspiracy!" and accused Google of punishing him for his support for "natural health" and Donald Trump. The truth appears to be that Adams violated one of Google's rules, leaving the question: What's the best way to fight fake news and fake medicine on the Internet?

Prove the scientific consensus and win a prize: A time-dishonored PR ploy used by cranks, quacks, and pseudoscientists (Robert F. Kennedy Jr. edition)
Last week, antivaccine activist Robert F. Kennedy, Jr. teamed up with Robert De Niro to issue a challenge to provide one scientific study that proves thimerosal in vaccines is safe, with a cash prize of $100,000. They thus joined a long line of antivaxers, creationists, and climate science denialists offering money to "prove" the scientific consensus. Science doesn't work that way.
In 2017, are antivaxers winning?
The election of Donald Trump as President has emboldened antivaxers, because they quite rightly sense that he is one of them. His inauguration as President, combined with other trends, have led observers to ask the question: Are antivaxers winning, or will 2017 be the year of the antivaxer?

Robert F. Kennedy, Jr. promotes an awful epidemiology study linking vaccines and neurological conditions from…Yale?
Robert F. Kennedy, Jr. has never seen a lousy study linking vaccines to bad things that he didn't like. This is no exception. Oddly enough, this study was funded and carried out by a lawyer and an investment banker, with the help of an eminent Yale pediatrician. Of course, the study doesn't show what RFK Jr. thinks it shows.
Donald Trump versus the FDA: Is the standard of evidence for drug approval actually too low rather than too high?
All of the candidates being considered by President Trump for FDA Commissioner believe that the FDA is too strict in its standards for approving new drugs. In a commentary in Nature last week, two bioethicists argued that, at least in terms of preclinical data, the standard of evidence is actually too low. Which is correct?

“Detox”: Ritual purification masquerading as medicine and wellness
If the "central dogma" of alternative medicine is that wishing makes it so, one of the most important of the other organizing dogmas of alternative medicine is that "toxins," whether they come from inside or outside, are making us sick and that we can't be healthy until we "detoxify." This is far more a religious belief than a science-based one.

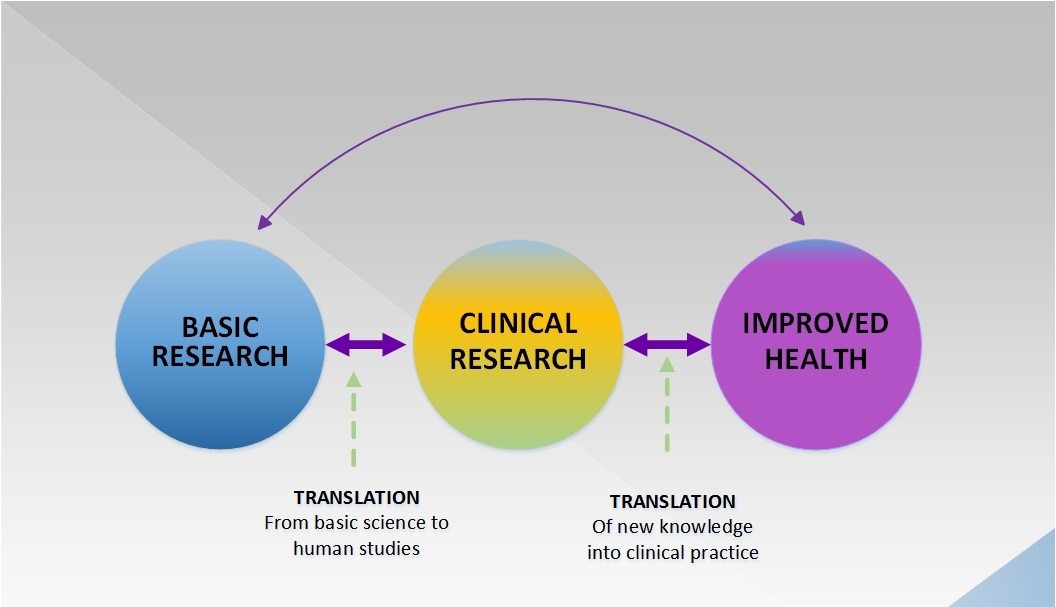
How reproducible is basic lab research in cancer biology?
Last week, a review of the reproducibility of several highly cited cancer biology papers was published. The results were mixed and demonstrate how difficult reproducing published results can be at times—and how scientists need to do better.

