Category: Cancer
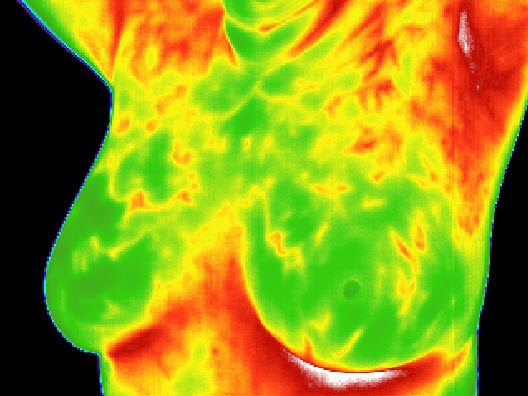
FDA issues warning letter to “holistic” practitioner offering thermography for breast cancer detection
Thermography for breast cancer detection is one of more than 65 products the FDA just announced it is going after for fraudulently claiming to prevent, diagnose, treat or cure cancer.

Contrary to what we are frequently told, we are not “losing the war on cancer”
A common narrative about cancer is that we are making no progress in our fight against it. Fortunately, the actual data do not agree. Yes, too many people still die of cancer and progress is slow, but it's not correct to claim that we are losing the war on cancer.

Did cannabis oil save Deryn Blackwell, the “boy in seven billion,” when his bone marrow transplant for two cancers was failing?
In a forthcoming book The Boy in 7 Billion, Callie Blackwell claims that cannabis oil, which she had started giving her son Deryn to relieve his symptoms during a bone marrow transplant for two cancers, actually saved his life when the bone marrow transplant appeared to be failing. Unfortunately, her story appears to be another testimonial that confuses correlation with causation.

The Texas Medical Board lets Stanislaw Burzynski off lightly: A cautionary tale of the failure of regulating medicine
After three years and countless twists and turns, the final decision by the Texas Medical Board on the sanctions to be imposed on Houston cancer quack Dr. Stanislaw Burzynski were announced on Friday. Sadly, they were not enough. The Burzynski saga should serve as a cautionary tale that the regulation of physicians and medicine is too lax, not too strict.

Why Do Things That Are Unlikely to Harm Us Get the Most Attention?
We are very bad at assessing risk, often giving the most attention to the things that are least likely to harm us. Geoffrey Kabat's new book teaches us how to think more clearly about scientific studies of environmental health risks.

Google delists Mike Adams’ Natural News website. Was it because of fake news?
Last week, in a surprise move Google delisted Mike Adams' Natural News website. Predictably, Adams immediately cried "Conspiracy!" and accused Google of punishing him for his support for "natural health" and Donald Trump. The truth appears to be that Adams violated one of Google's rules, leaving the question: What's the best way to fight fake news and fake medicine on the Internet?

Corrigendum. The Week in Review for 02/19/2017
More poorly done acupuncture studies. Burzynski eats just desserts. Italians like homeopathy. New Jersey is going after Oregon. And more
Corrigendum. The week in review for 02/12/2017
The week in review. Chiropractic and stroke. Integrative Medical doctors don’t trust vaccines. Death from medical marijuana. Shilajit: compost or mulch oozing from Himalayan rocks. India goes full Tuskeegee with AIDS. And more!

“Detox”: Ritual purification masquerading as medicine and wellness
If the "central dogma" of alternative medicine is that wishing makes it so, one of the most important of the other organizing dogmas of alternative medicine is that "toxins," whether they come from inside or outside, are making us sick and that we can't be healthy until we "detoxify." This is far more a religious belief than a science-based one.