Category: Clinical Trials
Curse Removal from the Annals. More Acupuncture Nonsense.
A short post this week. Last weekend was a busy call weekend and as I type this I am heading for Palm Springs for a long weekend of hiking in the desert. If there is no entry in 14 days, look for my bleached bones somewhere in Joshua Tree. Some observations about a recent article in the once-respected Annals of Internal Medicine,...
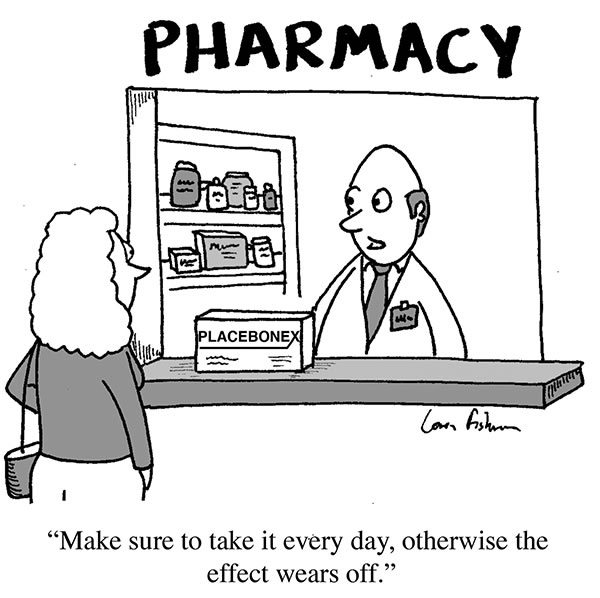
Is “harnessing the power of placebo” worthwhile to treat anything?
We frequently write about placebo effects here on Science-Based Medicine. The reason is simple. They are an important topic in medicine and, at least as importantly, understanding placebo effects is critical to understanding the exaggerated claims of advocates of “complementary and alternative medicine” (CAM), now more frequently called “integrative medicine” (i.e., integrating pseudoscience with science). Over the years, I (and, of course,...
The fine line between quality improvement and medical research
As I’ve mentioned before, the single biggest difference between science-based medicine (SBM) and what I like to call pseudoscience-based medicine, namely the vast majority of what passes for “complementary and alternative medicine” (CAM) or “integrative medicine” is that SBM makes an active effort to improve. It seeks to improve efficacy of care by doing basic and clinical research. Then it seeks to...
Is scientific peer review a “sacred cow” ready to be slaughtered?
I’ve frequently noted that one of the things most detested by quacks and promoters of pseudoscience is peer review. Creationists hate peer review. HIV/AIDS denialists hate it. Anti-vaccine cranks like those at Age of Autism hate it. Indeed, as a friend of mine, Mark Hoofnagle, pointed out several years ago, pseudoscientists and cranks of all stripes hate it. There’s a reason for...
Worshiping at the altar of the Cult of the Brave Maverick Doctor
One of my favorite television shows right now is The Knick, as I described before in a post about medical history. To give you an idea of how much I’m into The Knick, I’ll tell you that I signed up for Cinemax for three months just for that one show. (After its second season finale airs next Friday, I’ll drop Cinemax until...

Misinterpreting TACT: No, Chelation Does Not Outperform Statins for Heart Disease
Chelation with intravenous EDTA (disodium ethylene diamine tetra-acetic acid) has long been used for heavy metal poisoning. It binds the metal ions and facilitates their excretion from the body. In recent years it has been used for many other indications that are not evidence-based, such as autism and coronary heart disease. The Trial to Assess Chelation Therapy (TACT) was done to assess...
Exercise and Memory
There is no escaping the evidence that regular moderate exercise is associated with a host of medical benefits. Among those benefits are perhaps improved memory and cognition, and questionably a decreased risk of developing dementia. The latest study to show this correlation involved younger and older adults who wore a step-monitor. The number of steps they took during the study interval was...
Acupuncture/TCPM Crapfest
As I get older I get more grumpy. Issues that at one time I was rather sanguine about, now irritate the hell out of me. It is not like it was when I started practice. Information was hard to come by. Going through the Index Medicus, with the world’s tiniest font, wandering the stacks looking for papers, sending off for reprints, getting...
The elusive “potential” of integrative medicine
UPDATE: Dr. Katz has responded to this post in his usual venue, The Huffington Post. Alternative medicine was all about “potential” from the get go: In 1991, the Senate Appropriations Committee responsible for funding the National Institutes of Health (NIH) declared itself “not satisfied that the conventional medical community as symbolized at the NIH has fully explored the potential that exists in...

