Category: Clinical Trials

The evolving story of the harms of anti-inflammatory drugs
Owing to summer vacation, today’s post updates a 2011 post and a 2013 post with some new information. Anti-inflammatory drugs are among the most well-loved products in the modern medicine cabinet. They can provide good pain control, reduce inflammation, and eliminate fever. We give non-steroidal anti-inflammatory drugs (NSAIDs) in infancy, continuing through childhood and then adulthood for the aches and pains of...
Ethical Failures
It is summer vacation for me in Eastern Oregon at Sunriver. Unbelievable geology, fantastic hikes, great biking, wonderful golf, delicious beer and good food. The thesaurus fails me for superlatives. It is hard to get too riled up about all things SCAM to produce a blog entry when I could be doing one or all of the above. I really...

Update on Cholesterol and Statins
The consensus of mainstream medicine is that a high blood level of LDL cholesterol is a major risk factor for cardiovascular disease and that lowering high levels can help with prevention and treatment. Statins have been proven effective for lowering cholesterol levels and for decreasing cardiovascular and all-cause mortality. I recently wrote about the new guidelines for statin therapy. Currently half of...
Chiropractic and Stroke: The question is not answered
I am off to Chicago for 5 days to wow the SMACC crowd with my ID/SBM acumen. I hope. Given that most of my multiple-personalities do not seem to be able to get any work done, I am forced to write a brief post this week, limited by the battery life on my MacBook Air. Whatever I get down on paper? pixels?...
Homeopathic industry and its acolytes make poor showing before FDA
On April 21 and 22, the FDA held a public hearing: to obtain information and comments from stakeholders about the current use of human drug and biological products labeled as homeopathic, as well as the Agency’s regulatory framework for such products. . . . FDA is seeking participants for the public hearing and written comments from all interested parties, including, but not...

As in 2014, “right-to-try” laws continue to metastasize in 2015, part 2
"Right-to-try" laws sound on the surface to be reasonable and compassionate. They are neither. And they continue to metastasize from state to state.
Should placebos be used in randomized controlled trials of surgical interventions?
Trials of new experimental drugs frequently compare them to placebo, particularly when there is a large subjective component to the disease being treated, such as pain. In contrast, placebo-controlled trials are rarely undertaken in surgery, mainly because it's been considered ethically dicey to do sham surgery on one group. Should this change? Should we be more open to doing randomized, placebo-controlled surgery...

As in 2014, “right-to-try” laws continue to metastasize in 2015
Last year, I did several posts on what I consider to be a profoundly misguided and potentially harmful type of law known as “right-to-try.” Beginning about a year and a half ago, promoted by the libertarian think tank known as the Goldwater Institute, right-to-try laws began popping up in state legislatures, which I likened to Dallas Buyers Club laws. Both Jann Bellamy...
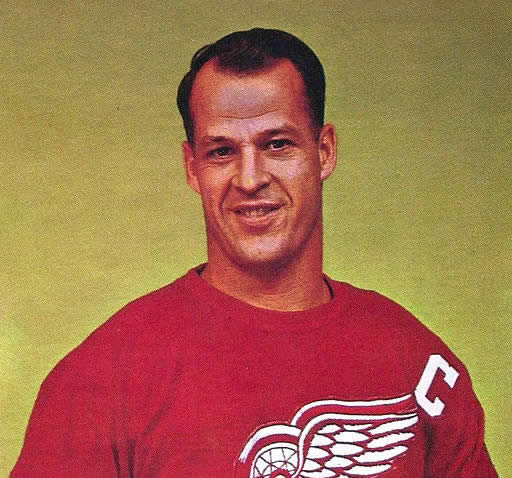
Stem cells versus Gordie Howe’s stroke, part 3
Here I am in Philadelphia attending the 2015 American Association for Cancer Research (AACR) meeting to imbibe the latest basic and translational science about oncology. So what am I doing in my non-conference time? I’m holed up in my hotel room near Rittenhouse Square writing a DoD Grant and this post. Fortunately, I am nearly done with the grant, with nothing I...
Anesthesia-Assisted Rapid Opioid Detox
Opioids are widely available as prescription drugs for pain: hydrocodone (e.g., Vicodin), oxycodone (e.g., OxyContin, Percocet), morphine (e.g., Kadian, Avinza), and codeine. Heroin, which has no medically approved use, is also an opioid. Unfortunately, opioids are also widely abused. How enticing it is to imagine a magic bullet for opioid drug addiction. Addiction causes huge social problems. Yet it is hard to...

