Category: Clinical Trials
Acupuncture for Withdrawal Symptoms in Critically Ill Infants
The practice of medicine, particularly our pharmaceutical and surgical interventions, involves a constant struggle between risk and benefit. If the physiology or anatomy of the human body is altered, even with the best of intentions, there is always a potential downside. There are certainly instances where the risk to benefit ratio is extremely favorable or unfavorable and the right recommendation is obvious,...

Stem cells versus Gordie Howe’s stroke, part 2
Another Christmas has come and gone, surprisingly fast, as always. I had thought that it might make a good “last of 2014” post—well, last of 2014 for me, anyway; Harriet and Steve, at least, will be posting before 2014 ends—to do an end of year list of the best and worst of the year. Unfortunately, there remains a pressing issue that doesn’t...
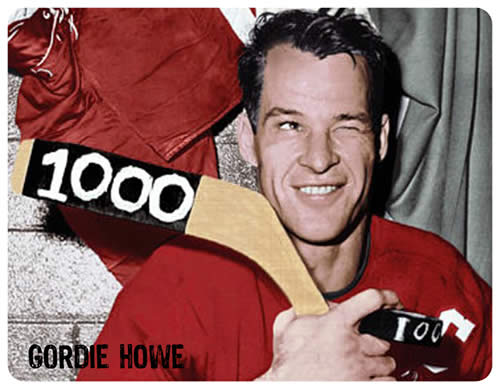
Stem cells versus Gordie Howe’s stroke
Note: There is now a major update to this story published here, which explains a lot of the questions remaining in this blog post. Seven years ago I returned to Michigan, where I was born and spent the first quarter century of my life, after an absence of more than 20 years. In the interim, I had done my surgical residency and...
Study of “Acupressure” for Constipation
A recent study in the Journal of General Internal Medicine evaluated a treatment for constipation. It tested whether training patients to massage the perineum (the area between the vagina or scrotum and the anus) would improve their reported bowel function and quality of life at 4 weeks after training. They found that it did. It’s a simple, innocuous treatment that may be...

Selling “integrative oncology” as a monograph in JNCI
The Society of Integrative Oncology publishes its "evidence-based" guidelines for the supportive care of breast cancer patients, along with a whole lot of musings on integrating quackery with medicine. But are the guidelines science-based? I think you know the answer to that one.

Eminent Harvard psychologist, mother of positive psychology, New Age quack?
Be less curious about people and more curious about ideas. – Marie Curie’s advice to journalists Harvard psychologist Ellen Langer was on CBS This Morning News explaining plans for a psychosocial intervention study with women with Stage IV metastatic breast cancer. The project would attempt to shrink women’s tumors by shifting their mental perspective back to before they were diagnosed. Seeing her...

Retconning the story of traditional Chinese medicine
Proponents of "integrating" traditional Chinese medicine (TCM) into medicine paint a tale of an ancient, unified system of medicine that's been tested over at least two millennia and found to be effective. The real story is very different and is best explained with a term more commonly used to discuss comic books. Basically, the "integration" of TCM into "Western medicine" is nothing...

Conspiracy theories and Ebola virus transmission
Yesterday, I spiffed up a post that some of you might have seen, describing how a particular medical conspiracy theory has dire consequences in terms of promoting non-science-based medical policy. Specifically, I referred to how the myth that there are all sorts of “cures” for deadly and even terminal diseases that are being kept from you by an overweening fascistic FDA’s insistence...

Using the fear of Ebola to promote the placebo legislation that is “right to try”
Libertarians and free market fundamentalists generally detest the FDA and want to dramatically decrease its power in the belief that the free market can guarantee the safety of drugs better than a government agency that requires strong scientific evidence of efficacy and safety before approval. Not surprisingly, they're at it again, this time in the service of promoting "right-to-try" laws and using...
Lessons from the dubious rise and inevitable fall of green coffee beans
News this week that a randomized controlled trial of green coffee bean (GCB) has been officially retracted from the medical literature signals what is hopefully the end to one of the most questionable diet products to appear on the market in years. Plucked from obscurity and then subjected to bogus research, it’s now clear that the only people that actually benefited from...

