Category: Clinical Trials
Lessons from the dubious rise and inevitable fall of green coffee beans
News this week that a randomized controlled trial of green coffee bean (GCB) has been officially retracted from the medical literature signals what is hopefully the end to one of the most questionable diet products to appear on the market in years. Plucked from obscurity and then subjected to bogus research, it’s now clear that the only people that actually benefited from...
Do doctors pay attention to negative randomized clinical trials?
We at the Science-Based Medicine blog believe that all medicine, regardless of where it comes from, should be held to a single science-based standard with regards to efficacy, effectiveness, and safety. We tend to focus primarily on “complementary and alternative medicine” (CAM), now more commonly known as “integrative medicine,” because (1) we believe it to be undermining the scientific basis of medicine...

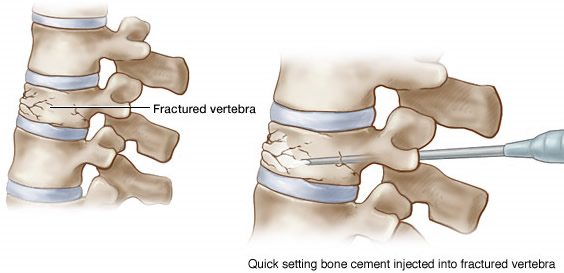
That’s so Chiropractic
Old bad studies: Fantastical autopsy results I found the following quote at “Chiropractic care can treat more than just bad backs” (FYI. Chiropractic can’t): Luse references a study published in The Medical Times authored by Dr. Henry Windsor [sic], M.D. that showcases the correlation of spinal health to overall wellness. Windsor dissected 75 human cadavers to investigate their causes of death. The...
Tens of millions for CAM research — and it’s all on your dime
The Federal Funding Accountability and Transparency Act (FFATA) was signed on September 26, 2006. The intent is to empower every American with the ability to hold the government accountable for each spending decision. The end result is to reduce wasteful spending in the government. The FFATA legislation requires information on federal awards (federal financial assistance and expenditures) be made available to the...
Clinical trials of integrative medicine: testing whether magic works?
I just thought that I’d take the editor’s (and, speaking for Steve, the founder’s) prerogative to promote our own efforts. Regular readers of SBM are familiar with our message with respect to randomized clinical trials of highly implausible “complementary and alternative medicine” treatments, such as homeopathy or reiki. Well, believe it or not, Steve and I managed to get a commentary...
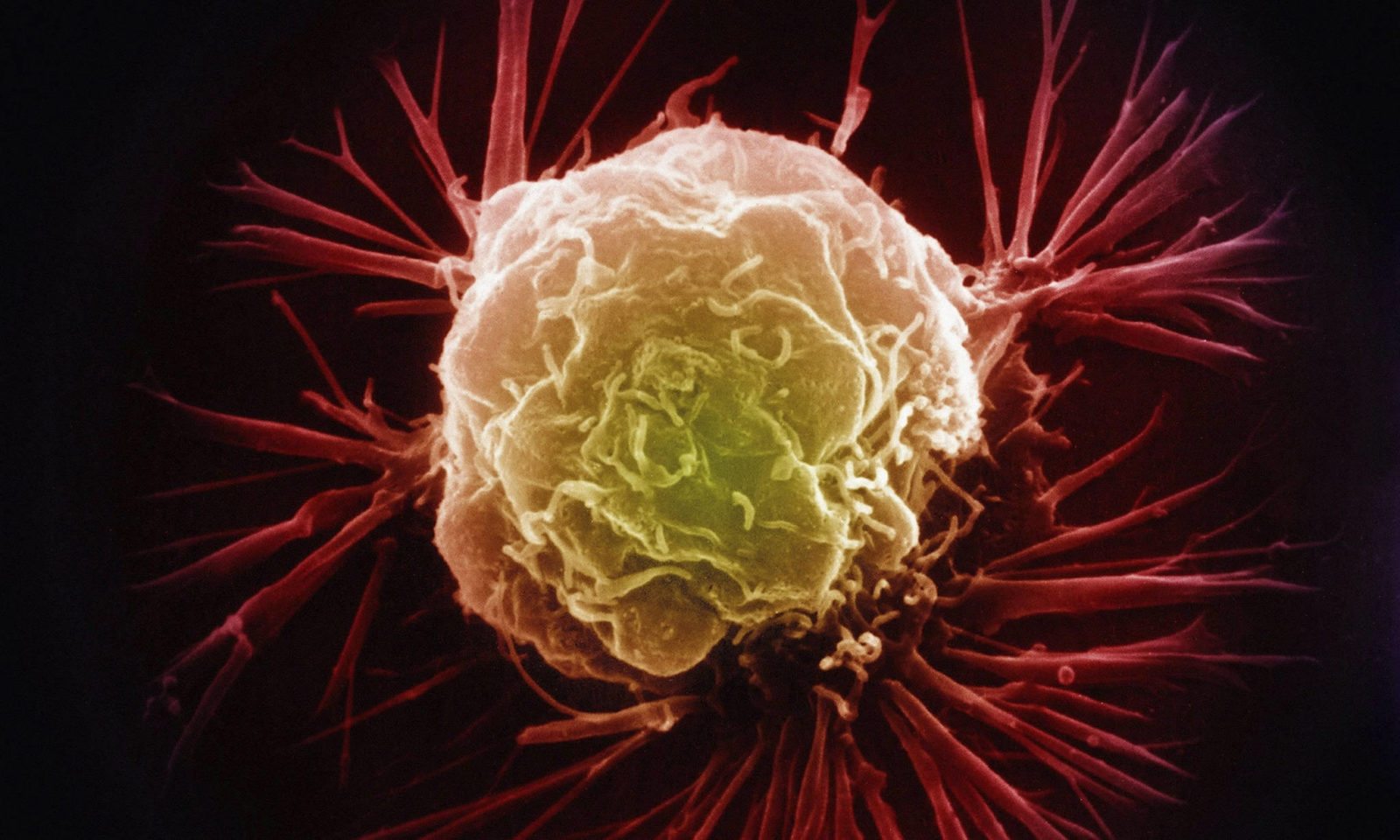
“Atavistic oncology” revisited: Dr. Frank Arguello responds
Three weeks ago, I wrote about a cancer treatment promoted by Dr. Frank Arguello that I deemed to be quackery, launching into one of my usual discussions based in science (and with a touch of snark) regarding why. Dr. Arguello, it appears, is not very happy about what I wrote. So he responded. He also sent e-mails complaining to my cancer center...

The Texas Medical Board vs. Stanislaw Burzynski, 2014 edition
Here we go again. I'll give the Texas Medical Board credit for one thing. It's persistent. It's going after Stanislaw Burzynski's medical license again. Will this finally be the time the TMB puts a stop to Burzynski's abuse of the clinical trial process and patients? Or will this be a replay of the 1990s, with Burzynski slithering away yet again?
Consortium of Academic Health Centers for Integrative Medicine research conference disappoints even NCCAM
In May, the International Research Congress on Integrative Medicine and Health (IRCIMH) conference was held in Miami. In the words of its website, the conference was “convened by” the Consortium of Academic Health Centers for Integrative Medicine (CAHCIM), “in association with” the International Society for Complementary Medicine Research. As CAHCIM chirped in this tweet: “Three days, 22 countries, 100 academic medical institutions,...

The Center for Inquiry weighs in on the FDA’s mishandling of Stanislaw Burzynski’s clinical trials
The Center for Inquiry points out how what Stanislaw Burzynski is doing corrupts the clinical trial process and harms patients.

Beware The P-Value
The p-value was meant to be used as a convenient and quick test to evaluate how likely a result was due to chance, or a real effect. It has since come to be treated as an indication of importance or truth, particularly in the CAM world. This is a problem.

