Category: Clinical Trials

Virtual Reality Therapy
Are virtual reality headsets a valid tool for treating back pain? Maybe.
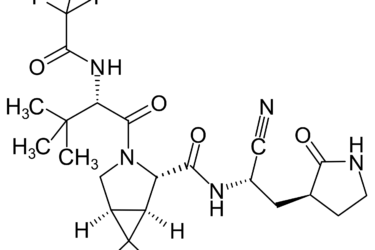
Pfizer’s new COVID-19 protease inhibitor drug is not just “repackaged ivermectin”
Pfizer recently announced that its new protease inhibitor-based drug was 89% effective in preventing hospitalization due to COVID-19 and it is seeking an emergency use authorization for it from the FDA. Antivaxxers claim that ivermectin targets the same protease and is being "suppressed" to protect Pfizer's profits from the new drug. What's the real story? Hint: Antivaxxers took a grain of truth...

What the heck happened to The BMJ?
Last week, The BMJ published an "exposé" by Paul Thacker alleging patient unblinding, data falsification, and other wrongdoing by a company running three sites for the massive clinical trial of the Pfizer COVID-19 vaccine. It was a highly biased story embraced by antivaxxers, with a deceptively framed narrative and claims not placed into proper context, leading me to look into the broader...
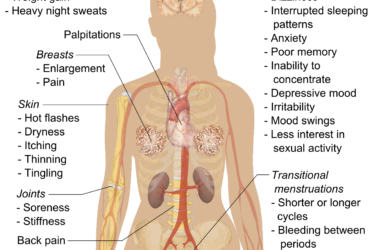
Laser Therapy for Vaginal Rejuvenation
Some doctors are offering laser therapy for "vaginal rejuvenation". It is no more effective than placebo, can cause harm, and is very expensive.

Ivermectin is the new hydroxychloroquine, take 6: Incompetence and fraud everywhere!
Ivermectin is the new hydroxychloroquine, a drug repurposed for COVID-19 that almost certainly doesn't work but is still being touted as a "miracle cure" by quacks, grifters, and political ideologues. Are the data supporting it all fraud?

Preventing Malaria: A Glimmer of Hope?
A recent clinical trial tested a new approach to malaria prevention involving monoclonal antibodies.
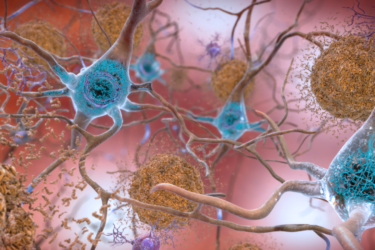
FDA’s Decision to Approve Aduhelm (aducanumab) for Alzheimer’s
Criticism of the FDA's decision to approve aducanumab for Alzheimer's disease.