Category: Diagnostic tests & procedures
Functional medicine: The ultimate misnomer in the world of integrative medicine
Functional medicine. It sounds so...scientific and reasonable. It's anything but. In fact, functional medicine combines the worst features of conventional medicine with a heapin' helpin' of quackery.
Regulating CAM Aussie Style
CAM proponents view National Health Interview Surveys recording the supposed popularity of CAM, an amorphous conflation of anything from conventional medical advice to mythical methods, as an invitation to unleash even more unproven remedies on the public. My interpretation is quite different. I see the same figures as proof that we are doing too little to protect the public from pseudoscience. In...
Carotid Artery Stenosis: Surgery, Stent, or Nonsurgical Stroke Prevention?
The carotid artery in the neck is a common site of atherosclerosis. As plaque builds up, it leaves less room for blood flow and can cause strokes through clotting or embolization. Carotid stenosis is defined as a greater than 70% narrowing of the lumen (the space through which the blood flows in an artery). It can cause symptoms, including transient ischemic attacks...
Health Savings Accounts: a tax-sheltered way to pay for quackery
If you want money to pay for pseudoscience, but your pesky health insurance company is getting in the way, a Health Savings Account might be just the solution. And if the Health Savings Act of 2016, sponsored by the Big Supplement’s own Senator Orrin Hatch, becomes law, your opportunities will be greatly expanded. First, let’s take a look at Health Savings Accounts...
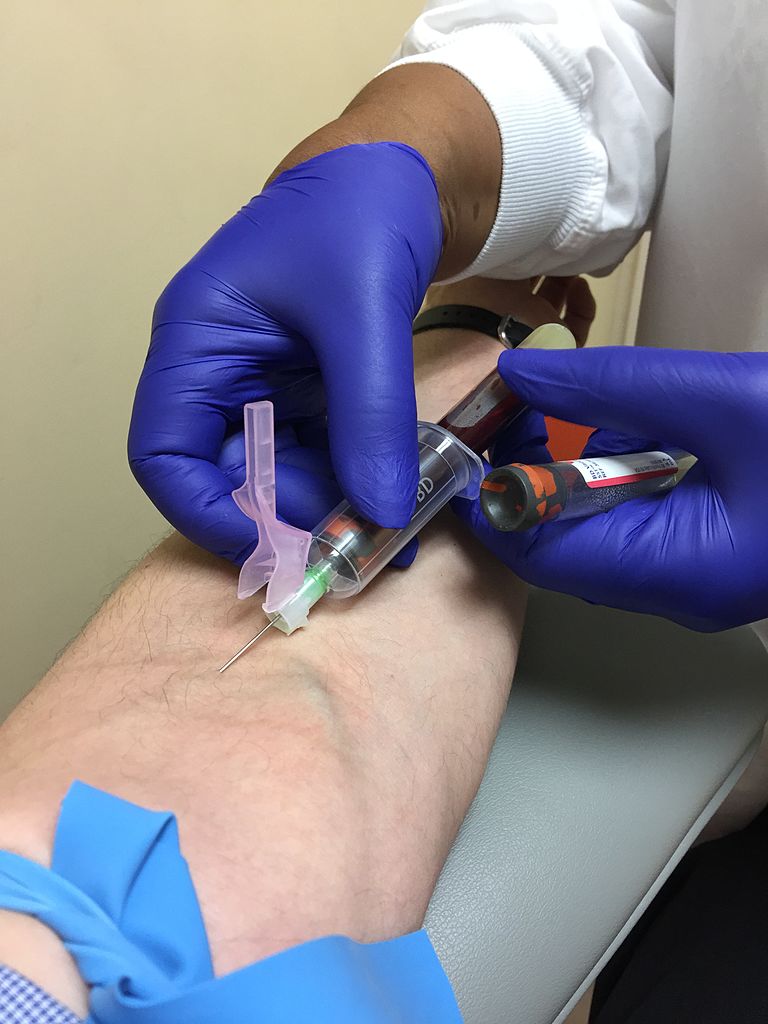
Lyme Testing
I hate those oh hell moments. I was up way too late last night, but who can pass up the opportunity to see Patti Smith playing Horses (and more) for the 40th anniversary of the album. Only 44? Behind the Eagles? No way. I would nudge it up a few more spaces. Hard to believe I was 18 when that album came...
Legislative Alchemy 2015: Another losing season for CAM practitioners
One of the main, but perhaps underappreciated, reasons quackery thrives in the United States is that the states legalize it by licensing practitioners of pseudoscience as health care providers. These practitioners are placed under the regulatory jurisdiction of, well, themselves. I call the whole deplorable process Legislative Alchemy, and you can see all posts on the topic here. It gives practitioners an...
Colonoscopy: More Misinformation from Mercola
Joseph Mercola, D.O., runs the website mercola.com which is full of misinformation, advocates all kinds of questionable alternative treatments including homeopathy, and discourages vaccination and other aspects of conventional medicine. Like Dr. Oz and Andrew Weil, he is more dangerous than easily recognizable quacks in that he combines some good medical information with egregious misinformation, and readers who know he is right...
Breast Milk Testing: Scaremongering, Not Science
New mothers, especially first-time mothers, tend to worry about whether they are doing what is best for their babies. A new service, Happy Vitals, will only add to those worries. We know that breast is best, but these folks make women question whether their breast milk is good enough. They say: Happy Vitals provides families with the tools they need to monitor...
“Liquid biopsies” for cancer screening: Life-saving tests, or overdiagnosis and overtreatment taken to a new level?
I’ve written many times about how the relationship between the early detection of cancer and decreased mortality from cancer is not nearly as straightforward as the average person—even the average doctor—thinks, the first time being in the very first year of this blog’s existence. Since then, the complexities and overpromising of various screening modalities designed to detect disease at an early, asymptomatic...
Here be Dragons: Caring for Children in a Dangerous Sea of sCAM
As a pediatrician working in a relatively sCAM-inclined region, it is not uncommon to find myself taking care of patients who are also being followed by so-called alternative medicine practitioners. This often creates a major obstacle to providing appropriate care and establishing an atmosphere of mutual trust in the provider-patient/parent relationship. It usually makes me feel like I’m battling invisible serpents in...

