Category: Medical Ethics
Dummy Medicines, Dummy Doctors, and a Dummy Degree, Part 1: a Curious Editorial Choice for the New England Journal of Medicine
Background This post concerns the recent article in the New England Journal of Medicine (NEJM) titled “Active Albuterol or Placebo, Sham Acupuncture, or No Intervention in Asthma.” It was ably reviewed by Dr. Gorski on Monday, so I will merely summarize its findings: of the three interventions used—inhaled albuterol (a bronchodilator), a placebo inhaler designed to mimic albuterol, or ‘sham acupuncture’—only albuterol...
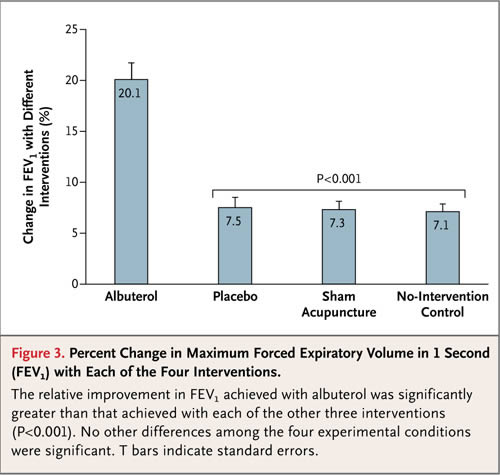
Spin City: Using placebos to evaluate objective and subjective responses in asthma
As I type this, I’m on an airplane flying home from The Amazing Meeting 9 in Las Vegas. Sadly, I couldn’t stay for Sunday; my day job calls as I’ll be hosting a visiting professor. However, I can say—and with considerable justification, I believe—that out little portion of TAM mirrored the bigger picture in that it was a big success. Attendance at...
“CAM” Education in Medical Schools—A Critical Opportunity Missed
Mea culpa to the max. I completely forgot that today is my day to post on SBM, so I’m going to have to cheat a little. Here is a link to a recent article by yours truly that appeared on Virtual Mentor, an online ethics journal published by the AMA with major input from medical students. Note that I didn’t write the...
Blatant pro-alternative medicine propaganda in The Atlantic
Some of my fellow Science-Based Medicine (SBM) bloggers and I have been wondering lately what’s up with The Atlantic. It used to be one of my favorite magazines, so much so that I subscribed to it for roughly 25 years (and before that I used to read my mother’s copy). In general I enjoyed its mix of politics, culture, science, and other...
Placebos as Medicine: The Ethics of Homeopathy
Is it ever ethical to provide a placebo treatment? What about when that placebo is homeopathy? Last month I blogged about the frequency of placebo prescribing by physicians. I admitted my personal discomfort, stating I’d refuse to dispense any prescription that would require me to deceive the patient. The discussion continued in the comments, where opinions seemed to range from (I’m paraphrasing) ...
Anti-vaccine warriors vs. research ethics
Three weeks ago, the anti-vaccine movement took a swing for the fences and, as usual, made a mighty whiff that produced a breeze easily felt in the bleachers. In brief, a crew of anti-vaccine lawyers headed by Mary Holland, co-author of Vaccine Epidemic: How Corporate Greed, Biased Science, and Coercive Government Threaten Our Human Rights, Our Health, and Our Children, published a...
Placebo Prescriptions
Whether it’s acupuncture, homeopathy or the latest supplement, placebo effects can be difficult to distinguish from real effects. Today’s post sets aside the challenge of identifying placebo effects and look at how placebos are used in routine medical practice. I’ve been a pharmacist for almost 20 years, and have never seen a placebo in practice, where the patient was actively deceived by...

Asian Bear Bile Remedies: Traditional Medicine or Barbarism?
Imagine living 20 years spending 24 hours a day in a cage that tightly fits your body, not giving you room to stand up, stretch out, turn around, or move at all. Imagine that twice a day during these years you would have a metal catheter inserted into a hole which has been cut into your abdomen, allowing the catheter to easily...
Ethics in human experimentation in science-based medicine
Science-based medicine depends upon human experimentation. Scientists can do the most fantastic translational research in the world, starting with elegant hypotheses, tested through in vitro and biochemical experiments, after which they are tested in animals. They can understand disease mechanisms to the individual amino acid level in a protein or nucleotide in a DNA molecule. However, without human testing, they will never...
Of SBM and EBM Redux. Part IV: More Cochrane and a little Bayes
NB: This is a partial posting; I was up all night ‘on-call’ and too tired to continue. I’ll post the rest of the essay later… Review This is the fourth and final part of a series-within-a-series* inspired by statistician Steve Simon. Professor Simon had challenged the view, held by several bloggers here at SBM, that Evidence-Based Medicine (EBM) has been mostly inadequate...

