Category: Medical Ethics
Fake treatments for real diseases: A review of allergy and asthma advertisements by naturopaths, chiropractors, homeopaths and acupuncturists
A majority of Canadian chiropractic, naturopathic, homeopathic and acupuncture clinics claim that they can diagnose or treat allergies, sensitivities and asthma.
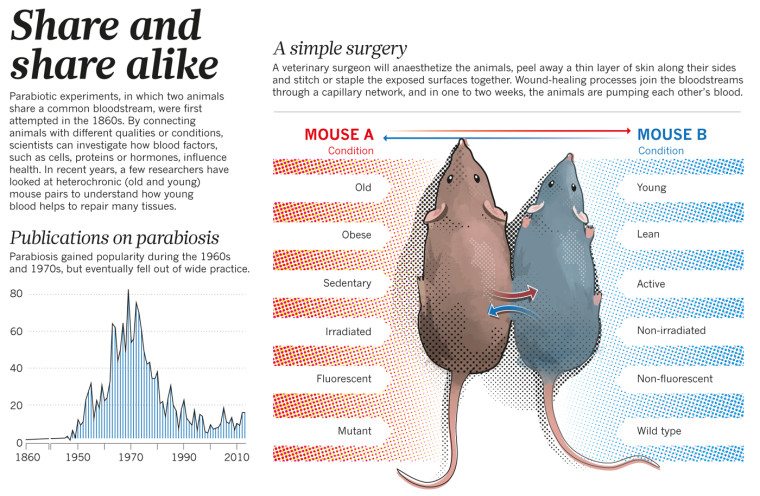
Parabiosis – The Next Snakeoil
The pattern has repeated so many times that it is truly predictable. Scientists turn their eyes to one type of treatment that has theoretical potential. However, proper research from theory to proven treatment can take 10-20 years, if all goes well. Most such treatments will not work out – they will fail somewhere along the way from the petri dish to the...

Forget stem cell tourism: Stem cell clinics in the US are plentiful
It's generally thought that quack stem cell clinics are primarily a problem overseas because the FDA would. never allow them on US soil. As a new survey shows, that assumption couldn't be more wrong.
Academic Consortium plan: force medical residents to practice integrative medicine
“Integrative medicine” (IM) is an ideological movement within medicine driven in large part by those whose livelihoods depend on its continued existence. This includes both those with positions in academic medicine and individual practitioners who use the IM brand to attract patients. Despite IM and its antecedents (alternative, complementary, alternative and complementary, complementary and integrative) having been around for about a quarter...
Is it ethical to sell complementary and alternative medicine?
Complementary and alternative medicine may be legal to sell - but is it ethical to sell?
The fine line between quality improvement and medical research
As I’ve mentioned before, the single biggest difference between science-based medicine (SBM) and what I like to call pseudoscience-based medicine, namely the vast majority of what passes for “complementary and alternative medicine” (CAM) or “integrative medicine” is that SBM makes an active effort to improve. It seeks to improve efficacy of care by doing basic and clinical research. Then it seeks to...
Worshiping at the altar of the Cult of the Brave Maverick Doctor
One of my favorite television shows right now is The Knick, as I described before in a post about medical history. To give you an idea of how much I’m into The Knick, I’ll tell you that I signed up for Cinemax for three months just for that one show. (After its second season finale airs next Friday, I’ll drop Cinemax until...
The Ethics of Prescribing Worthless Treatments
Is it ever ethical for a physician to prescribe a treatment to a patient that they know to be entirely without efficacy? Is it ever possible to do this without deceiving the patient to some degree? I think the answer to both questions is a clear “no.” Within the flipped reality of “alternative medicine,” however, it suddenly becomes acceptable to deceive patients...
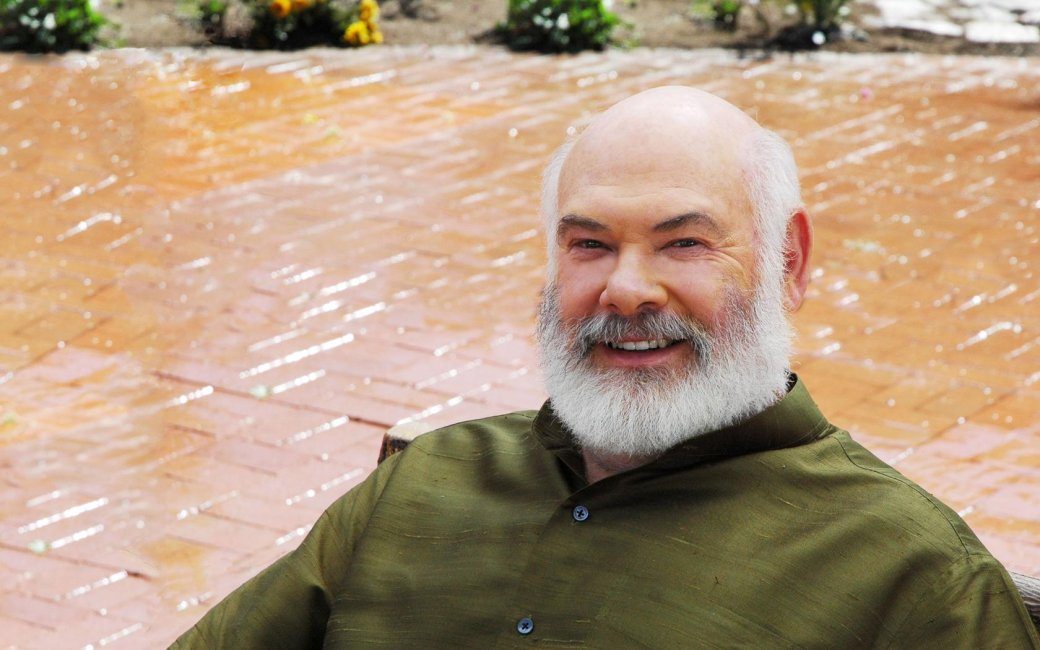
To debate or not to debate: The strange bedfellows of Andrew Weil
Those who stand on the wrong side of science love public debates and frequently challenge science advocates to them. The reason, of course, is that public debates are almost never a good venue to argue science, and these debates almost never happen in a truly neutral venue. This time around, I got a bit of ego gratification when Andrew Weil apparently wanted...
Learning quackery for Continuing Medical Education credit
The Integrative Addiction Conference 2015 (“A New Era in Natural Treatment”) starts tomorrow in Myrtle Beach, SC. Medical doctors, doctors of osteopathy, naturopaths and other health care providers will hear lectures on such subjects as “IV Therapies and Addiction Solutions,” given by Kenneth Proefrock, a naturopath whose Arizona Stem Cell Center specializes in autologous stem cell transplants derived from adipose tissue. Proefrock,...

