Category: Medical Ethics
Is Homeopathy Unethical?
“A gentle ethical defence of homeopathy” by Levy et al. was recently published in an ethics journal. A full-text preprint is available online. They say: Utilitarian critiques of homeopathy that are founded on unsophisticated notions of evidence, that adopt narrow perspectives on healthcare assessment, and that overstate the personal, social and ontological harms of homeopathy, add little to our understanding of the...
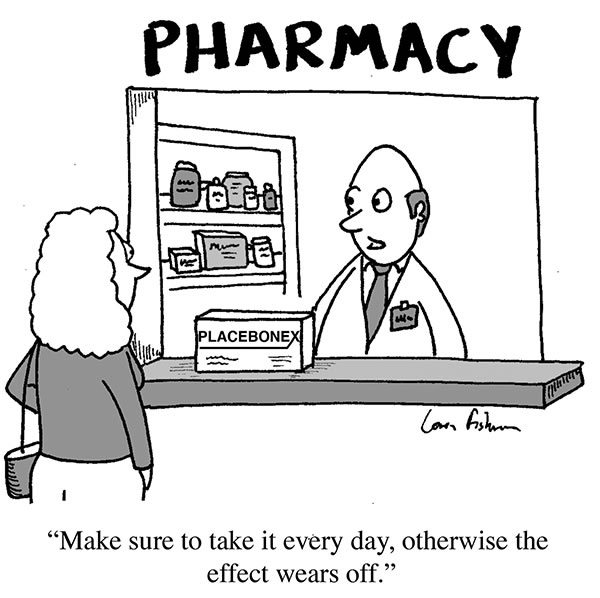
Placebo by Conditioning
Truly understanding placebo effects (note the plural) is critical to science-based medicine. Misconceptions about placebo effects are perhaps the common problem I encounter among otherwise-scientific professionals and science communicators. The persistence of these misconceptions is due partly to the fact that false beliefs about placebos, namely that “the” placebo effect is mainly an expectation mind-over-matter effect, is deeply embedded in the culture....
Don’t just stand there, do nothing! The difference between science-based medicine and quackery
The Merriam-Webster Dictionary defines science as: Knowledge about or study of the natural world based on facts learned through experiments and observation. And: Knowledge as distinguished from ignorance or misunderstanding. While this should distinguish science from pseudoscience, those who practice the latter often lay claim to the same definition. But one of the major differences between science and pseudoscience is that science...
Cancer Centers and Advertising Practices
You have probably seen the TV commercials or other ads for Cancer Treatment Centers of America. They make it sound like “the place to go” if you have cancer. They claim to be “different,” to combine the best cancer technologies with natural therapies in a humane, patient-centered approach that helps you fight the disease and maintain your quality of life. They offer...

The Wild West: Tales of a Naturopathic Ethical Review Board
In Arizona, a naturopathic institutional review board has been set up to examine the ethics of naturopathic research projects. It's going about as well as naturopathic training and practice.
Pseudoscience North: What’s happening to the University of Toronto?
Today’s post is a reluctant challenge. I’m nominating my own alma mater, the University of Toronto, as the new pseudoscience leader among large universities – not just in Canada, but all of North America. If you can identify a large university promoting or embracing more scientifically questionable activities, I’ll happily buy you a coffee. Yes, it’s personal to me, as I...
Significant Ruling Against Conversion Therapy
The standard features of quackery are all there. Proponents of this particular therapy claim that a normal condition is a disease. They make false claims about the cause of this disease. They then charge thousands of dollars for their fake treatment to cure the fake disease, and claim success rates that are not backed by any statistics. In this case the fake...
Facing Decline and Death
Note: Atul Gawande and his book will be featured on a Frontline episode airing on PBS tonight. We’re all going to die. (There’s nothing like starting on a positive note! 🙂 ) We’re all going to die, and if we are fortunate enough to survive long enough to become old, we’re all going to experience a decline of one sort or another...
Selling complementary and alternative medicine: An business ethics perspective
Is it ethical to sell complementary and alternative medicine? This presentation — by a philosopher and a pharmacist — considers CAM from the perspective of commercial ethics.
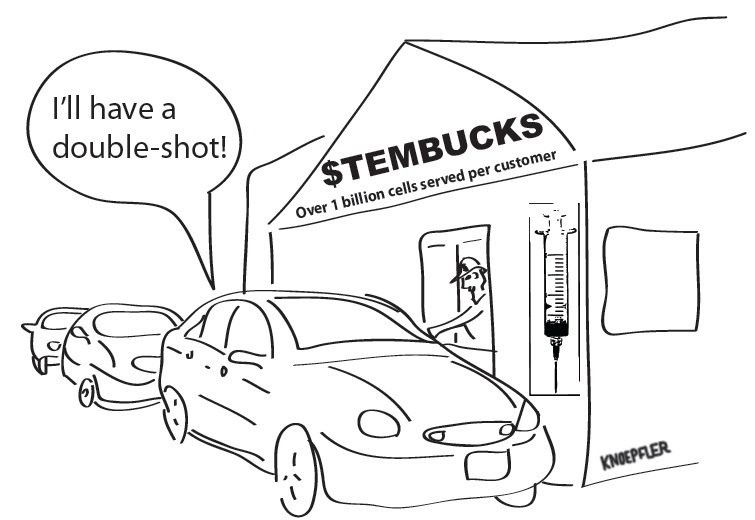
Stem cell clinics and unapproved, for-profit human experimentation
Editor’s note: I met Dr. Paul Knoepfler online in the wake of my two posts on Gordie Howe and his stem cell treatment for stroke. I was impressed by his posts on the topic and what I saw at his own blog. Given that he’s a stem cell researcher, I wanted him to write a post on stem cell clinics like the...

