Category: Medical Ethics

Stem cells versus Gordie Howe’s stroke, part 2
Another Christmas has come and gone, surprisingly fast, as always. I had thought that it might make a good “last of 2014” post—well, last of 2014 for me, anyway; Harriet and Steve, at least, will be posting before 2014 ends—to do an end of year list of the best and worst of the year. Unfortunately, there remains a pressing issue that doesn’t...
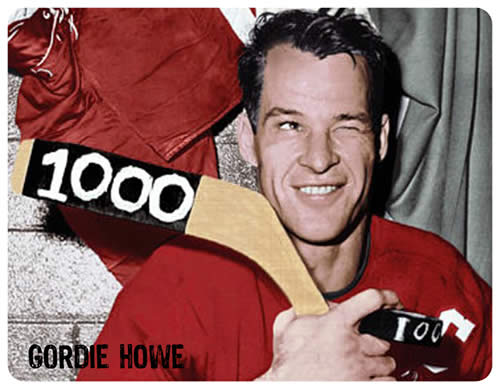
Stem cells versus Gordie Howe’s stroke
Note: There is now a major update to this story published here, which explains a lot of the questions remaining in this blog post. Seven years ago I returned to Michigan, where I was born and spent the first quarter century of my life, after an absence of more than 20 years. In the interim, I had done my surgical residency and...

Eminent Harvard psychologist, mother of positive psychology, New Age quack?
Be less curious about people and more curious about ideas. – Marie Curie’s advice to journalists Harvard psychologist Ellen Langer was on CBS This Morning News explaining plans for a psychosocial intervention study with women with Stage IV metastatic breast cancer. The project would attempt to shrink women’s tumors by shifting their mental perspective back to before they were diagnosed. Seeing her...
Legislating Ignorance
Science is under attack, and not just from anti-vaccine celebrities and parents with degrees from Google University. Scientific illiteracy is being woven into the very fabric of our society through legislative assault. If you dismiss this as alarmist hyperbole, you haven’t been paying close enough attention. Every day thousands of pediatric health care providers throughout the country provide safety advice to patients...
The false dichotomies of CAM and “integrative medicine”
A lot of medical specialties have throwaway newspapers/magazines that are supported by advertising and somehow mysteriously managed to show up for free in the mailboxes of practitioners. In my case, I’ve found myself on the subscription list for such papers about oncology, but also general surgery (I’m Board-certified as a general surgeon). When I have to recertify in about three years, it...
Should the Incidental Discovery of Nonparentage be Disclosed?
The July issue of Pediatrics, the official journal of the American Academy of Pediatrics, contains an extremely thought provoking article discussing the risks and benefits of disclosing an incidental finding of nonparentage during pediatric genetic testing. Nonparentage occurs when one, or very rarely both, of the social parents did not serve as source code for a child’s genetic programming, so to speak....
The Truth?
Summertime and the living is easy. I am in Sunriver, Oregon for the week and I though, hilariously, that I would have plenty of time to write a post. Between the hiking, the biking, the golf, the food and the beer, there has been little time to sit in from of a keyboard. There may be no better place to spend a...
Consortium of Academic Health Centers for Integrative Medicine research conference disappoints even NCCAM
In May, the International Research Congress on Integrative Medicine and Health (IRCIMH) conference was held in Miami. In the words of its website, the conference was “convened by” the Consortium of Academic Health Centers for Integrative Medicine (CAHCIM), “in association with” the International Society for Complementary Medicine Research. As CAHCIM chirped in this tweet: “Three days, 22 countries, 100 academic medical institutions,...
Dr. Oz and the Terrible, Horrible, No Good, Very Bad Day
Dr. Mehmet Oz is one of the most well-known, and possibly the most influential medical doctor in America. The Dr. Oz Show is broadcast in 118 countries and reaches over 3 million viewers in the USA alone. When Oz profiles a product or supplement on his show, sales explode – it’s called “The Dr. Oz Effect”. Regrettably, Oz routinely and consistently gives...

Reiki: Fraudulent Misrepresentation
The Center for Integrative Medicine at the Cleveland Clinic sells reiki treatments (also here) to patients with cancer, fertility issues, Parkinson’s Disease and digestive problems, as well as other diseases and conditions. The Center’s website ad describes reiki as a form of hands-on, natural healing that uses universal life force energy . . . [a] vital life force energy that flows through...

