Category: Politics and Regulation

Legislative Alchemy: Undaunted by rejection in 2020, naturopaths return to state legislatures seeking licensing and practice expansion
States largely rejected naturopathic licensing and practice expansion efforts in 2020. As ever, naturopaths are back again in 2021, imploring state legislators to legitimize them with licensing and greater scopes of practice, especially the authority to prescribe drugs.

Consumer and public health groups push for cancer warning on alcoholic beverages
A coalition of consumer and public health groups, citing scientific consensus, is pushing for a government-required warning that alcohol consumption causes cancer on alcoholic beverage containers. Despite the evidence, we can expect alcohol industry opposition.

Federal appeals court strikes down conversion therapy bans
A recent federal Court of Appeals decision struck down local governments' conversion therapy bans on First Amendment grounds, characterizing licensed mental health therapists' advice as a "viewpoint" and regulation thereof subject to strict scrutiny by the courts, a standard that, historically, is rarely met. This decision carries disturbing implications for the regulation of the practice of medicine as well as the government's...

Exploitation of Mammals for Traditional Remedies
A recent review hints at the extent to which endangered mammals are exploited for fake medicines.
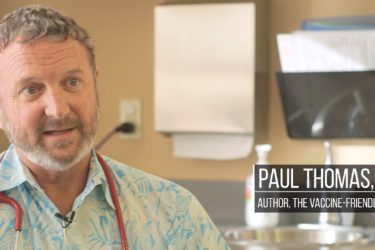
The Oregon Medical Board suspends the medical license of antivax pediatrician Dr. Paul Thomas
Late last week, the Oregon Medical Board suspended the licenses of two physicians, one for bragging about not wearing a mask around his patients, the second being Dr. Paul Thomas, an antivaccine pediatrician, whose continued practice was deemed a threat to his patients. It's time for more state medical boards to step up, as Oregon's has.

FDA and FTC issue more warning letters citing products and services making illegal COVID claims
The FDA and FTC have issued hundreds of warnings to companies selling products and services claiming, without adequate evidence, that they can prevent or treat COVID-19, but the possibility of government action doesn't seem to be a deterrence.
Joe Biden defeated Donald Trump. Now what for science-based medicine?
In 2016 and 2020, scientists expressed surprise and alarm at the results of the Presidential election. In 2016 it was alarm that someone as antiscience as Donald Trump was elected, and in 2020 it was over how close the election was, given Trump's dismal record on science, medicine, and the COVID-19 pandemic. Are scientists out of touch? And now what, for federal...
The Top COVID-19 Hucksters and Grifters…so far
It wouldn't be a health crisis without those that want to profit from it.

Vaccine safety monitoring in the age of the COVID-19 pandemic
Last year, the Trump administration essentially disbanded the National Vaccine Program Office, folding it into an office focused on infectious diseases. Then the COVID-19 pandemic hit. What does this mean for monitoring the safety of the soon-to-be-approved COVID-19 vaccines?

Government watchdog to investigate politicization of CDC and FDA during COVID-19 pandemic
Based on numerous reports of White House interference, a government watchdog will investigate politicization of the CDC's and FDA's actions during the coronavirus pandemic.

