Category: Politics and Regulation

Sensible Medicine: Medical Misinformation and Medical Groupthink From the Medical Establishment
We all have biases, including in-group loyalty. It's often easy to see such bias in others, though nearly impossible to see in oneself. As such, it's both normal and dangerous to imagine that only those who disagree with you are vulnerable to groupthink, while you are perfect beacon of independent, rational thought- along with everyone who agrees with you.

The American Board of Internal Medicine finally acts against two misinformation-spreading doctors
Last week, I wrote about how COVID-19 has exposed the toothlessness of state medical boards. Last week, the American Board of Internal Medicine announced that it was going to permanently revoke the board certifications of two COVID-19 contrarian doctors, Drs. Paul Marik and Pierre Kory. Can medical specialty boards make up for the failure of state medical boards, at least partially?

What’s really in that sports supplement?
A new analysis of sports supplements shows that you cannot trust the label to tell you what's actually in the bottle.

COVID-19 has exposed the toothlessness of state medical boards
A report in The Washington Post last week revealed just how badly state medical boards have been failing when dealing with physicians spreading COVID-19 misinformation and using quackery to prevent and treat the disease. None of this is anything new, unfortunately. The pandemic has merely stress tested state medical boards, and most have failed because of political choices made long ago.

RFK Jr.: A fart-filled argument gives way to an antisemitic conspiracy theory that COVID-19 is an “ethnically targeted” bioweapon
Last week, RFK Jr. endured hilariously bad press about an NYC press event at which two of his supporters argued over climate change, one with lots of farts. However, the fart jokes soon gave way to darker side of the event, a Q&A in which RFK Jr. shared an antisemitic conspiracy theory claiming that COVID-19 might have been "targeted" against Caucasians and...
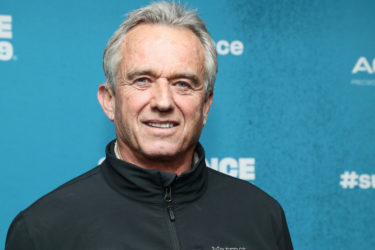
RFK Jr. resurrects an old antivax half-truth about “saline placebos” in randomized controlled trials of vaccines
Robert F. Kennedy, Jr. has resurrected the antivax claim that the childhood vaccine schedule has never been tested in randomized controlled trials (RCTs) with a saline placebo controls (and therefore the vaccine schedule is unsafe). This is an old and deceptive antivax half-truth that ignores both what constitutes a scientifically valid placebo and the ethical requirements for RCTs.
RFK Jr. and Joe Rogan: Putting the old denialist technique of bad faith “Debate me, bro!” challenges on steroids
Joe Rogan conveyed a challenge by antivax crank turned Presidential candidate RFK Jr. to vaccine scientist Dr. Peter Hotez to "debate me, bro!" In the week since, wealthy right wingers have added money to the inducement, and through an awful op-ed by Ross Douthat this weekend, even the New York Times has amped up the pressure for a "debate" about vaccines with...
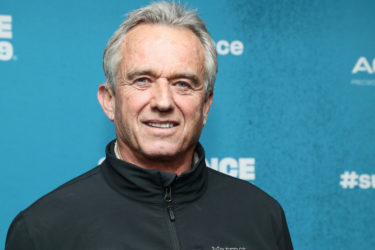
Is Robert F. Kennedy, Jr. antivaccine? Judge him by his own words!
Last week, an antivaxxer on Substack—where else?—tried to argue that Robert F. Kennedy, Jr. is not antivaccine by encouraging you to judge him by his own words. I agree. You should judge RFK Jr. by his own words, as they show definitively that he has been antivaccine since at least 2005.

Detransition, Retransition, and What Everyone Gets Wrong
A article published in The Atlantic implored people to take detransitioners seriously but did so by perpetuating non-evidence-based tropes that harm both detransitioners and transgender people

The (Cold) Drugs Don’t Work
The FDA continues to permit the inclusion of an ineffective ingredient in hundreds of cough and cold products.

