Category: Public Health

US Preventive Services Task Force Recommends Against Multivitamins
An updated review of the evidence reinforces that routine vitamin use is mostly worthless.

Medical debt vs. universal health insurance: The interface between SBM and policy
This blog has long argued that the best medicine is science-based medicine (SBM). The problem is that in the US SBM is often not accessible, except at ruinous cost, which is why I argue that we have to broaden our definition of SBM to include the systems that deliver it and pay for it.

Justin Bieber, Ramsay Hunt syndrome, SADS, and how to antivaxxers everything is always about vaccines
I never thought I'd be writing about Justin Bieber, but such are the strange times we live in, given how after Bieber announced that he had developed facial paralysis as a result of Ramsay Hunt syndrome antivaxxers swooped in to blame it on COVID-19 vaccines. Elsewhere, they blame every unexplained death of a young person on vaccines to the point of claiming...

Do Covid-19 Vaccines Affect Fertility?
Fears of future infertility are keeping some parents from vaccinating their children for COVID-19. These fears are not supported by any evidence.
Should We Fear the Monkeypox?
A recent outbreak of monkeypox is likely containable, but people are understandably concerned.
Ayn Rand, Objectivists, and COVID
Healthcare workers are leaving medicine after coming under attack due to the type of disinformation spread by Objectivists. That's ironic.

Vaccines Don’t Save Lives
Fostering basic critical thinking skills and countering medical misinformation is a vital undertaking.

Yes. I Remember it Well. A COVID 45 Retrospective
With faltering memory, questionable opinions, and sketchy references, an infectious disease revenant reflects on the last 2.5 years of COVID 45. Grizzly bear assault free. As in no assault, not the price of a Grizzly bear assault.
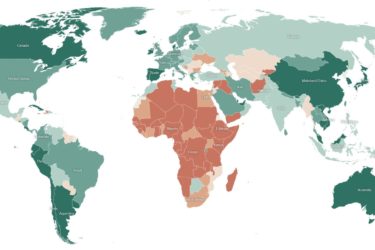
The Toll of COVID
We can't take our eyes off the ball just yet - what's the state of the pandemic?

Vitamin D for the prevention of COVID-19: A randomized controlled trial
A large clinical trial shows vitamin D supplementation had no effect on COVID-19.

