Category: Science and Medicine
Misinformation and disinformation about facemasks and COVID-19
As evidence accumulates that facemasks work to decrease the risk of spreading COVID-19, new myths have arisen claiming that, not only do facemasks not work, but that they are actively harmful. These myths have no basis in physiology or chemistry, but that hasn't stopped anti-mask activists from using them to claim protection under the Americans With Disabilities Act.

Lotus Birth To Blame for Death of Australian Newborn
Lotus Birth, an "ethically inadmissible" practice where a newborn is left attached to the placenta for several days, is risky, benefit free, and is likely to blame for the death of an Australian infant in 2017.
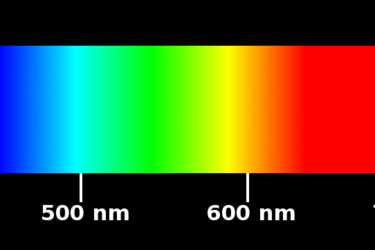
Blue light blocking glasses: How much of the hype is science-based?
Blue light from our electronics is said to be harmful, and "blue blocking" glasses are touted as a panacea to numerous health issues. Is there any evidence to substantiate these claims?
J.B. Handley’s unthinking person’s guide to the COVID-19 pandemic
J.B. Handley was the founder of the antivaccine group Generation Rescue. Unfortunately, in the era of COVID-19 he's started peddling pseudoscience related to the pandemic. Some things never change.

Should We Avoid Dairy Out of Fear of Cancer?
A doctor is adamant about avoiding dairy because IGF-1 allows cancer cells to multiply. I think he's relying on speculation and an over-abundance of caution.

A Rare and Mysterious Inflammatory Syndrome in Children is Linked to COVID-19
A mysterious inflammatory condition, likely caused by COVID-19, is affecting a small number of children. We don't know much about it yet, but we are certain to see additional cases and to learn more about why this is happening. Still, it's not time to panic.
Antivaxxers launch a preemptive disinformation war against a COVID-19 vaccine that doesn’t yet exist
We don't yet have a vaccine against COVID-19, but that hasn't stopped the antivaccine movement from launching a preemptive disinformation war on social media against it. Unfortunately, as a recent study demonstrates, on Facebook at least, they have been so successful that it is possible that antivaccine messaging will surpass pro-vaccine messaging on FB within a decade.

Smoking and COVID
Does smoking worsen COVID infections? Or is it protective? As more evidence emerges, the smoke is starting to clear.
COVID-19: Out-of-control science and bypassing science-based medicine
During the COVID-19 pandemic, there hasn't just been a pandemic of coronavirus-caused disease. There's also a pandemic of misinformation and bad science. It turns out that doctors today are just as prone as doctors 100 years ago during the 1918-19 influenza pandemic to bypass science-based medicine in their desperation to treat patients.


Do face masks decrease the risk of COVID-19 transmission?
As wearing masks to prevent the spread of COVID-19 becomes a culture war issue, the evidence for whether they prevent transmission of COVID-19 remains contested. A new systematic review and meta-analysis provides the best evidence yet that social distancing and masks are highly effective at decreasing the risk of contracting coronavirus, while eye protection might also help, but it's not a slam...