Category: Science and Medicine

(Dys-)Functional Medicine Comes to Dentistry
The great philosopher Deepak Chopra wrote: “I do not believe in meaningless coincidences. I believe every coincidence is a message, a clue about a particular facet of our lives that requires our attention.” So when SBM author extraordinaire Jann Bellamy emailed me last week with an article about so-called “Functional Dentistry” with the comment “Blog fodder?”, I looked it over with interest...

Medical Theater: Vaccines and Ebola
And all the men and women merely players; They have their exits and their entrances, And one man in his time plays many parts, His acts being seven ages. At first, the infant, Mewling and puking in the nurse’s arms. Then the whining schoolboy, with his satchel And shining morning face, creeping like snail Unwillingly to school. And then the lover, Sighing...
New Study on Homeopathic Cough Syrup for Children Reveals a Lack of Effectiveness and Ethics
On the pages of SBM we frequently discuss homeopathy, and rightfully so considering its position as one of the most pervasive yet dumbest forms of alternative medicine. Just yesterday our own Scott Gavura, who is neither pervasive nor dumb, wrote an excellent review of some recent improvements in the regulation of these ridiculous remedies in Canada, and I encourage readers to check...
A homeopathic win for consumers
Do you believe in magic? It might surprise you to learn that some people believe sugar pills have healing properties. This belief system, called homeopathy, is a multi-billion dollar industry worldwide, and it’s growing. While there is no convincing evidence to demonstrate that homeopathic treatments are more effective than a placebo, many consumers and even some health professionals accept homeopathy as a...
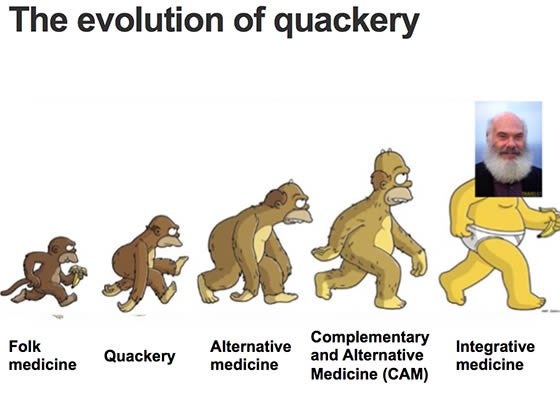
We Should Abandon the Concept of “Alternative Medicine”
In a recent editorial for the New York Times, Aaron E. Carroll argues, “Labels Like ‘Alternative Medicine’ Don’t Matter. The Science Does.” I agree with this headline thesis, but the details of his argument ironically show the harm that the so-called CAM (complementary and alternative medicine) movement has done. Carroll starts out well, essentially pointing out that the division between “conventional” and...
About that Cell Phone and Cancer Study
Recently there was another round of scaremongering headlines and articles claiming that cell phones can cause brain cancer. The Daily News wrote: “The scientists were right — your cell phone can give you cancer.” Many online news sites declared: “SHOCK STUDY: CELLPHONES CAN CAUSE CANCER,” in all caps to make sure you understand that you should be alarmed. None of the mainstream...
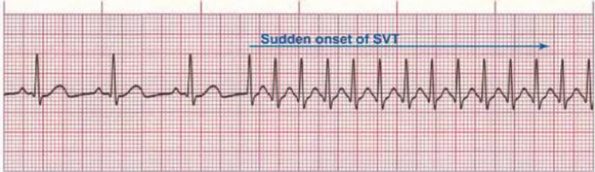
Neck Adjustment for Newborn Supraventricular Tachycardia: More Chiropractic Manipulation of Reality…..
[Editor’s note: Not enough Clay for one day? Check out this post on homeopathy over at The Scientific Parent!] It was recently brought to my attention that a chiropractor was promoting his profession on Facebook by claiming to have treated and cured a potentially life-threatening cardiac arrhythmia. The condition in question, supraventricular tachycardia (SVT), can be very serious and even deadly in...
Rehydrating with an appeal to nature
I don’t tend to worry too much about hydration, except when I exercise. I’ve been running regularly for over 15 years, and since I started I’ve usually carried water, or for longer runs, I drink old-school Gatorade. The formulation is basic: sugar, salt, and potassium. There are hundreds of electrolyte products marketed for athletics, but I’ve been faithful to the original: It’s...
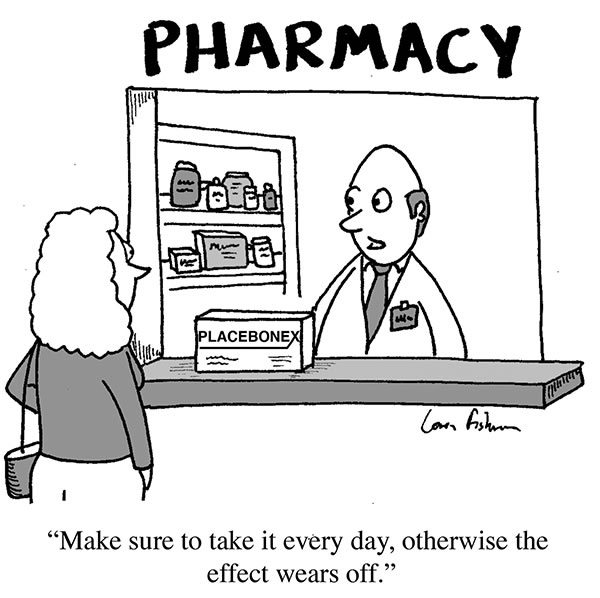
Placebo by Conditioning
Truly understanding placebo effects (note the plural) is critical to science-based medicine. Misconceptions about placebo effects are perhaps the common problem I encounter among otherwise-scientific professionals and science communicators. The persistence of these misconceptions is due partly to the fact that false beliefs about placebos, namely that “the” placebo effect is mainly an expectation mind-over-matter effect, is deeply embedded in the culture....


