Category: Surgical Procedures

On “integrative medicine” and walking and chewing gum at the same time
Evidence matters. Science matters. However, when advocates of "integrating" quackery into medicine via the vehicle of "integrative medicine" invoke weak science and poor quality evidence in conventional medicine in response to criticism, what they are really doing is deflecting attention away from their quackery. More importantly, advocates of science-based medicine are capable of walking and chewing gum at the same time. We...
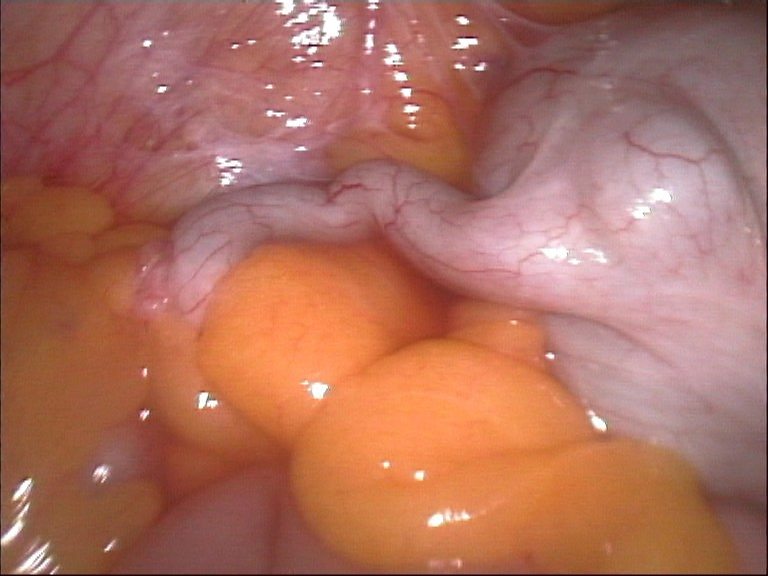
An Alternative to Appendectomy: Antibiotics
My title doesn’t refer to alternative medicine, it refers to an alternative within medicine: treating appendicitis with antibiotics instead of surgery. You may be surprised to learn that patients with appendicitis don’t always automatically need an appendectomy. A recent randomized controlled trial in Finland compared surgery to medical treatment. History of appendicitis treatment There is an excellent, detailed history of appendicitis available...
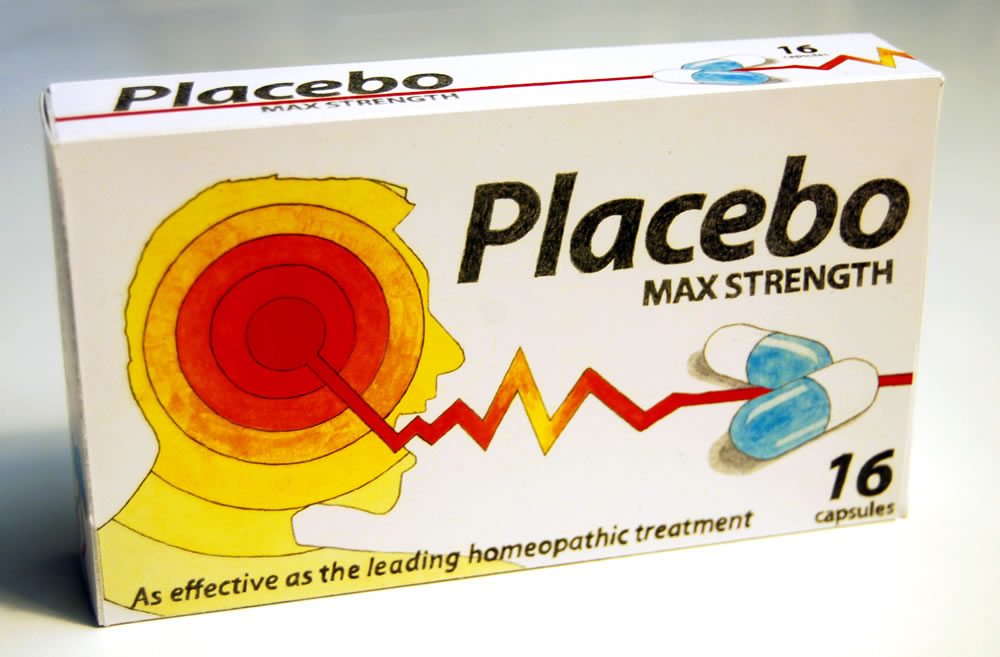
Should placebos be used in randomized controlled trials of surgical interventions?
Trials of new experimental drugs frequently compare them to placebo, particularly when there is a large subjective component to the disease being treated, such as pain. In contrast, placebo-controlled trials are rarely undertaken in surgery, mainly because it's been considered ethically dicey to do sham surgery on one group. Should this change? Should we be more open to doing randomized, placebo-controlled surgery...
Angelina Jolie, surgical strategies for cancer prevention, and genetics denialism (revisited)
Sometimes, weird things happen when I’m at meetings. For example, I just got home from the Society of Surgical Oncology (SSO) meeting in Houston over the weekend. Now, one thing I like about this meeting is that, unlike so many other meetings these days—cough, cough, ASCO, I’m looking at you—at the SSO there wasn’t a single talk I could find about “complementary...
The Marvelous Dr. Mütter
The Mütter Museum in Philadelphia has a marvelous collection of human bones, surgical specimens, monsters in jars, and medical memorabilia. It holds attractions for everyone, from the jaded medical professionals who thought they’d seen it all to the coveys of youngsters who compete to point out the grossest items to their friends, from the student of history to the connoisseur of the...

Medicine past, present, and future: Star Trek versus Dr. Kildare and The Knick
I love the new Cinemax series The Knick, which is set in 1900 and portrays a brilliant maverick surgeon named Dr. John Thackery on the cutting edge of medicine at the time. I also love Star Trek's Dr. "Bones" McCoy and have recently come to like the old radio show featuring Dr. Kildare. Looking at how the three shows portray medicine in...
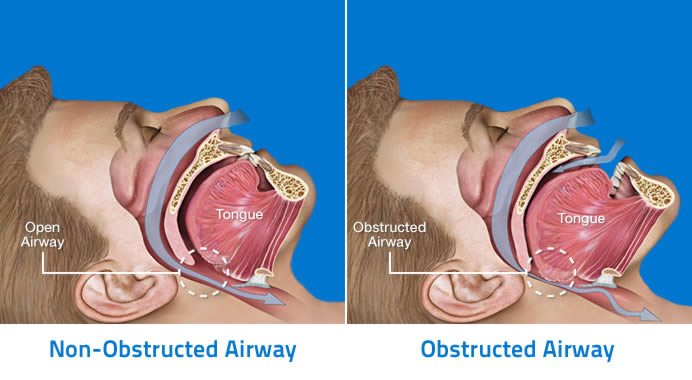
Dental Management Of Obstructive Sleep Apnea
[Editor’s Note: I’m pleased to announce that Grant Ritchey has agreed to join SBM as a regular. He’ll be writing about dental science and pseudoscience every four weeks on Sunday. (I swear, we’ll get up to seven day a week publishing if it kills me—or the other bloggers.) Grant will be starting with science, but I’m sure he’ll soon be discussing all...
Science-based medicine throughout time
As 2013 comes to a close, because this probably will be my last post of 2013 (unless, of course, something comes up that I can’t resist blogging about before my next turn a week from now), I had thought of doing one of those cheesy end-of-year lists related to the topic of science-based medicine. Unfortunately, I couldn’t come up with anything I...
On humility, confidence, and science-based surgery
Every so often, the reality of trying to maintain a career in science-based medicine interferes with the fun that is writing for this blog. Basically, what happened is that I spent the entire weekend working on three different grant applications and, by the time Sunday night rolled around, I was too exhausted to write what I had originally planned on writing. Fortunately,...
Knee Osteoarthritis: Thumbs Down for Acupuncture and Glucosamine
One more time: acupuncture and glucosamine are useless for osteoarthritis.

