Even though yesterday was Easter, and, as unreligious as I am, I was still thinking of taking it easy, there was one target that popped up that I just couldn’t resist. My wife and I were sitting around yesterday reading the Sunday papers and perusing the Internet (as is frequently our wont on Sunday mornings), when I heard a contemptuous harrumph coming from her direction. She then pointed me to an article in our local newspaper entitled Gluten-free beauty products in demand among some customers. Now, I must admit that I haven’t been keeping up with the gluten-free trend, other than how easily it fits within the niche of “autism biomed” quackery, where, apparently, nearly every “biomed” protocol for autistic children demands that gluten be stripped completely from their diets, lest the evil molecule continue to infect them with the dreaded autism. I’ve kept an eye the literature, but haven’t really written about gluten. That’s why I could immediately tell why my wife had called my attention to the article:
Amy Soergel’s lip gloss was making her sick. The problem, she realized, was gluten — hydrologized wheat protein, to be exact. Then she went to the hairdresser who used a shampoo that made her neck burn. Again, it contained gluten.
“There’s hidden gluten in many places you may not consider,” including stamp and envelope glues, toothpaste and lip balms, said Soergel, who has a store, Naturally Soergel’s, near Pittsburgh that caters to people with allergies. Indeed, for people with celiac disease, a bit of gluten that might get swallowed from a lipstick or a stream of shampoo in the shower can be enough to cause illness.
A slew of gluten-free skin care products have come on the market, including items from well-known companies such as Murad, Dr. Hauschka, EO, MyChelle, Suntegrity, Acure and derma-e. Many are sold in Whole Foods and other health food stores. If they’ve been certified by a third-party agency, an icon usually appears on the packaging.
Whole Foods. Of course, it had to be Whole Foods (among others). Let’s take a look at the whole gluten-free movement and then at the end I’ll revisit the question of gluten-free cosmetics and skin products.
Gluten, of course, is nothing more than proteins found in wheat endosperm (a type of tissue produced in seeds and that is ground to produce flour) and can also be found in barley and rye. It consists of two proteins, gliadin (a prolamin protein) and glutenin (a glutelin protein). Gluten cannot be consumed by sufferers of celiac disease (CD), whose main manifestation is inflammation of the bowel lining when gluten is eaten. The end result of this chronic inflammatory process can be gastrointestinal scarring and atrophy of the villi (the finger-like protrusions of the lining of the bowel responsible for nutrient absorption, among other things). The most common symptoms are, of course, gastrointestinal, including diarrhea, nausea, abdominal pain, and bloating, but CD can also manifest itself in a number of other symptoms, including skin rashes, weight loss and fatigue, oral ulcers, joint pain, anemia, and depression. CD (or gluten-sensitive enteropathy) is not caused by gluten, but rather a genetic predisposition. If you’re unlucky enough to have this predisposition, gluten can do bad things to you.
There is no doubt that CD can cause real problems in the people who have true gluten sensitivity. Indeed, as this New York Times article describes, in the 1990s the general medical consensus was that in the US the prevalence of CD was around 1 in 10,000. More recent studies, such as this one from 2012, report a prevalence of around 1 in 100. Worse, the majority of CD goes undiagnosed. In actuality, what is happening appears to be a combination of more intensive screening due to better awareness of celiac disease as a potential cause of puzzling symptom constellations, plus what is arguably a real increase in prevalence since 1950, estimated by Mayo Clinic researchers to be approximately four-fold and continuing to increase over the last decade.
The definitive diagnosis of CD is made by:
- Detection of anti-gluten antibodies in the blood (specifically, as Scott Gavura described, IgA antiendomysial antibody (EMA) and the IgA tTGA), a test that is 90-95% sensitive and 95% specific. This is suggestive of gluten-sensitive enteropathy but not fully diagnostic.
- The gold standard test: Distal duodenal biopsy specimens demonstrating characteristic histologic changes in the small intestinal mucosa, changes that include: a spectrum from total to partial villous atrophy and crypt lengthening with an increase in lamina propria and intraepithelial lymphocytes. It is also important to take at least six biopsies, because changes can be patchy.
It’s also noted in multiple sources that these tests should in general be done before the patient is placed on a gluten-free diet, because otherwise the tests often produce a false-negative result. There is also a controversial condition known as “non-celiac gluten sensitivity” (NCGS). As both Steve Novella and Scott Gavura note, these are patients without definitive diagnostic criteria for CD who believe that gluten causes symptoms of bloating, fatigue, and irritable bowel syndrome, but do not have antibodies to gliadin. Indeed, Scott quite correctly speculated over whether non-celiac gluten sensitivity is becoming the new Candida; i.e., an all-purpose bogeyman responsible for all sorts of vague, chronic health complaints and thus a nice foundation upon which quacks can base all sorts of dubious therapies related to removing gluten from the diets of anyone with vague complaints but no evidence of CD on testing.
Scott also noted the dearth of good studies on NCGS, and a review of PubMed just yesterday found that, although there are about 27 more articles out there in PubMed than there were when Scott last wrote about NCGS, the quality of evidence supporting the existence of the entity of NCGS remains poor. For example, in 2013, Biesiekierski et al. reported a placebo-controlled, cross-over rechallenge study of 37 subjects, in which they found no evidence of specific or dose-dependent effects of gluten in patients with NCGS placed on diets low in fermentable, oligo-, di-, monosaccharides, and polyols (FODMAPs) in order to control other potential triggers of gut symptoms. No markers of intestinal injury were noted in any of the groups, although a high nocebo response was noted. It’s not surprising that a recent review article characterized NCGS as “an entity awaiting validation, better diagnostic criteria, and, if it does exist, pathogenic mechanisms.” It was also noted that the “reluctance to acknowledge other components of wheat, such as fructans, non-gluten proteins and WGA, as potential pathogenic factors has often hampered good interpretation of clinical observations.” In other words, people are so fixated on gluten that they ignore other potential components of wheat and grains that might be the real cause of symptoms noted. The authors of the review article even go so far as to propose reasonable rules for future rigorous clinical trials on the subject:
Essential rules for future studies should include the following. First, celiac disease has to be seriously excluded by HLA studies and/or strict histological and immunological criteria. The inclusion of patients with intraepithelial lymphocytosis will always raise the issue of whether they really have celiac disease with a milder intestinal lesion. Secondly, the use of blinded placebo-controlled food re-challenge methodology to prove gluten sensitivity is present is not reliable, especially in patients who believe they have NCGS. Perhaps the selection of patients for study should be those with IBS naïve to a GFD. Thirdly, the trap of assuming that response to a GFD or exacerbation of symptoms due to a gluten-containing diet reflects specific effects of gluten should be outlawed and credence be given to the other wheat-related food constituents that can also cause gastrointestinal symptoms. Perhaps if these rules were followed, we would now be a lot closer to defining mechanisms by which gluten might act, might have developed biomarkers to identify patients who truly do have NCGS and perhaps, most importantly, answered the question of whether NCGS does really exist. On current evidence the existence of the entity of NCGS remains unsubstantiated.
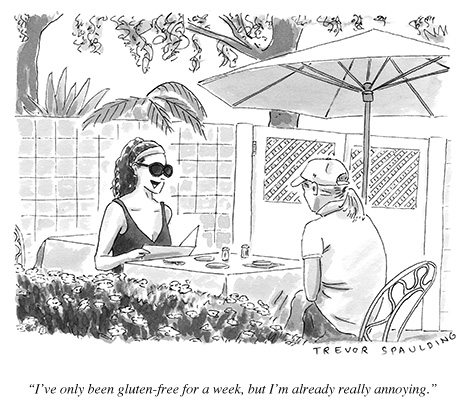
So, in other words, CD is a real entity that is more common that diagnosed, but it is not even clear whether NCGS is a distinct clinical entity, despite the number of people who believe themselves to have it, the number of companies that cater to the belief that this entity exists, and the number of practitioners, particularly “integrative” practitioners and alternative practitioners, who have come up with all sorts of exclusionary diets and “biomedical” interventions to treat it. As yet, we do not have convincing, reproducible clinical evidence that the condition exists, which makes it premature to be speculating about mechanisms, no matter how much advocates of gluten-free diets as a cure-all for everything might “draw a line in the sand” and try to dismiss skeptics who don’t cite the biomarker studies they like as they promote dubious “paleo” diets. Does any of this mean that NCGS doesn’t exist or is bogus? No, not necessarily. What it means is that evidence is inconclusive and contradictory. Worse, because of relentless messaging in popular culture that gluten is bad for you, that many—who knows how many?—people have undiagnosed gluten sensitivities, and that most people would be better off without gluten in their diets, there’s a substantial nocebo effect. Meanwhile, confirmation bias, nocebo and placebo effects, regression to the mean, and the usual confounders that make individual experience so unreliable when determining if an intervention is effective in an individual explain the vast majority of glowing “testimonials” of people who “go gluten-free” and believe it made them so much healthier. Here’s a perfect example of An Open Letter to Gluten-Free Skeptics:
I gave up gluten in 2010. At the time I had no symptoms of gluten sensitivity – no digestive issues, no overt symptoms of problems. No diagnosis of celiac. I was, however, obese (and have been for most of my life), and prone to uncontrollable binge eating. I gave it up as an experiment – not sure that it would help me, just hoping.
And it did.
I’ve been leaner, and generally healthier, during the past 3 years than at any prior time in my life. And this hasn’t been an easy 3 years – it’s been very stressful (for reasons having nothing to do with food), yet despite lots of travel and lots of serious life changes, I’ve been able to lose most of my excess fat and keep it off, without very much effort.
This was not my first attempt at leaning out – I’ve tried many different eating strategies, from low fat to low carb to vegetarianism to intermittent fasting – over the years. None of them “stuck” until I went gluten free.
He continues:
Even if I DON”T have dozens of double blind studies published in peer reviewed journals showing that a GF intervention reduces inflammation, improves digestion, and leads to weight loss, I DO have evidence that it vastly improved MY life and health.
And:
But as much as YOUR argument that I don’t have science proving gluten is bad for everybody – nobody has any science showing that NOBODY benefits from a GF diet.
Let me reiterate: NOBODY has ever done even a single study that shows in any sense that NOBODY benefits from eliminating gluten from their diet.
None of which demonstrates that a gluten-free diet did anything for this man. These are, in fact, the same sorts of arguments, confusing correlation with causation riddled with confirmation bias that antivaccinationists use to “prove” that vaccines cause autism, that “autism biomed” can “recover” autistic children, and even that Stanislaw Burzynski or Robert O. Young cured their cancers. They prove little or nothing. Unfortunately, given the panoply of vague symptoms attributed to NCGS, it’s a condition, if it exists, that’s seemingly custom-made for all the confounders that make demonstrating the efficacy of a treatment so difficult. That’s why the rules suggested in the review article I cited above are so critical to future studies. Unfortunately, it’s also why gluten is likely to continue to be demonized beyond its health effects on people who have true CD.
Which brings us back to why on earth anyone thinks gluten-free cosmetics and beauty products are of any value. The answer is: They aren’t, with possibly one exception. The reason, of course, is that the gluten protein is too large to be absorbed through the skin. Now, it is known that it only takes a relatively small amount of gluten ingestion to result in gastrointestinal problems, as little as 50 mg (present in 1/80th of a slice of wheat bread) can cause damage to the intestinal villi. Consequently, there is a rationale for “going gluten-free” for any product that goes on the lips or in the mouth, such as lip balm, toothpaste, or lipstick, at least for people with severe CD. For people who think they have NCGS, where it hasn’t even been convincingly demonstrated that gluten is actually the component in wheat that causes symptoms, gluten-free cosmetics is nothing but marketing hype feeding into the same marketing hype behind the gluten-free products that are only really needed by people who have true CD and only debatably helpful to others. Remember, as I’ve seen pointed out, 93% of consumers purchasing gluten-free products are not diagnosed with CD, but rather do so because of an interest in “health and wellness,” ascetic-based practices of self-improvement, or the “flavor of the month” diet trend.
But what about gluten-free skin products? In general, these are an even bigger waste of money, again because gluten isn’t absorbed through the skin. Most of the reports, like this one, in which people attribute skin issues to gluten, do not constitute decent evidence that topical gluten causes their symptoms. The reason is simple. Those with CD not-infrequently suffer from dermatitis herpetiformis, a type of skin rash, as part of their symptoms, that is not caused by contact with gluten (indeed, a gluten skin patch test is notoriously poor in sensitivity for diagnosing CD) but by ingesting gluten. When they remove gluten from their diet, their dermatitis herpetiformis resolves with the rest of their symptoms. Such people, once they are made aware that they have CD, start wondering if gluten in skin products can be the cause. Not surprisingly, they switch to gluten-free skin products at the same time they are removing gluten from their diet, and, as usually happens, their skin symptoms recede along with their gastrointestinal symptoms.
But what about the rest, who do not have CD but buy gluten-free skin products in order to avoid rashes? In my estimation, they’re wasting their money if they’re paying a premium for such products. If they’re not paying a premium, than it’s how well the product works for them that matters, not whether it has gluten in it or not. Again, there are many compounds and substances in skin products that can cause allergic reactions or simply contact dermatitis in some people, particularly fragrances. Because of all the publicity about gluten, it’s not surprising that so many people, whether they have CD or not, are quick to assume that a rash after using a skin product is due to gluten in the product. Without careful patch testing, assuming a reaction is due to gluten in a skin product is a leap.
It’s become clear that, up until the last decade or so, CD was severely underdiagnosed in the US. To some extent, it still is, although increased awareness and better-defined diagnostic criteria have alleviated that problem. Unfortunately, it is also a condition that appears to be increasing in prevalence, both due to an apparent increase due to greater awareness and, thus, diagnosis and, likely, to an increase in the actual frequency, as evidenced by studies suggesting that the prevalence of seropositivity for the appropriate IgA antibody in the population. In general, increased awareness is a good thing, as it allows for the appropriate diagnosis and treatment of a greater fraction of people with CD. So is the increased availability of gluten-free options for the approximately 1% of the population with CD, which allows them to alter their diet without suffering as grievous a hit to their quality of life.
Unfortunately, the known deleterious health effects of gluten in people with CD have been extrapolated into a much vaguer, as-yet scientifically unvalidated, clinical entity that supposedly a much larger percentage of the population suffers from. This has led to the unjustified demonization of gluten (which is really only harmful in a small minority of the population), overblown claims for “going gluten-free,” and ridiculous products such as gluten-free skin care products, deodorants, and shampoos.