[Editor’s note: It’s a holiday here in the U.S.; consequently, here is a “rerun” from my other super not-so-secret other blog. It’s not a complete rerun. I’ve tweaked it a bit. If you don’t read my other blog, it’s new to you. If you do, it’s partially new to you. See you all next week with brand spankin’ new material. It also (I hope) complement’s Scott’s excellent post from Thursday discussing the same issue and the same paper, but from a different perspective.]
As a cancer surgeon specializing in breast cancer, I have a particularly intense dislike reserved for cancer quacks, which I have a hard time containing at times when I see instances of such quackery applied to women with breast cancer. I make no apologies. These women are, after all, the type of patients I spend all my clinical time taking care of and to whose disease my research has been directed for the last 13 years or so. That’s why I keep revisiting the topic time and time again. Unfortunately, over the years, when it comes to this topic there’s been a depressing amount of blogging material. Indeed, Scott Gavura took a bite out of this particularly rotten apple just a few days ago. Even though he handled the discussion quite well, I thought it would be worthwhile for a breast cancer clinician to take a look. Our perspectives are, after all, different, and this is an issue that, from my perpective, almost can’t be discussed too often.
One question that comes up again and again is, “What’s the harm?” Basically, this question boils down to asking what, specifically, is the downside of choosing quackery over science-based medicine. In the case of breast cancer, the answer is: plenty. The price of foregoing effective therapy can be death; that almost goes without saying. In fact, it can be a horrific and painful death. It is, after all, cancer that we’re talking about. Aside from that, however, the question frequently comes up just how much a woman decreases her odds of survival by avoiding conventional therapy and choosing quackery. It’s actually a pretty hard question to answer. The reason is simple. It’s a very difficult topic to study because we as physicians have ethics. We can’t do a randomized trial assigning women to treatment or no treatment, treatment or quacke treatment, and then see which group lives longer and by how much. If a person can’t see how unethical that would be without my having to explain it, that person is probably beyond explanations. (As an aside, I can’t help but point out that a randomized trial of not vaccinating versus vaccinating is unethical for exactly the same reason; physicians can’t knowingly assign subjects to a group where he knows they will suffer harm. There has to be clinical equipoise.) There’s no doubt that foregoing effective treatment causes great harm.
So when it comes to figuring out just how much harm a woman risks by choosing quackery, all we’re left with, and rightfully so from an ethical standpoint, are lower quality studies, usually retrospective, and, fortunately, not very many of them. The reason is that they’re very hard to do, again because they’re retrospective and generally it’s hard to locate a sufficient number of women who turn down all surgery. The last time I discussed such a study was three years ago. It was a small study of only thirty three patients, but it found significantly decreased survival among the patients examined who eschewed conventional therapy in favor of “alternative” medicine. For example, five out of six patients who refused surgery progressed to stage IV metastatic disease, with a median time to being diagnosed with metastases of 14 months. Another study examining 5,339 women who refused surgery alone, but not necessarily other treatments, found that patients who refused surgery had a significantly decreased survival and a two-fold higher chance of dying of their disease.
Just this month, another such study was published in the World Journal of Surgical Oncology. It’s a study out of Alberta, specifically the University of Alberta and the Cross Cancer Institute and is entitled simply Outcome analysis of breast cancer patients who declined evidence-based treatment. Its design was relatively simple; it was a retrospective chart review of breast cancer patients who refused recommended treatments from 1980 to 2006. Patients who had “refused standard therapy” were defined thusly:
Any patient who has completely refused the recommended standard primary treatment plan following biopsy confirmation of breast cancer is considered as refusal of standard treatment. Primary treatment could be surgery, neoadjuvant radiotherapy or chemotherapy. Patients who refused adjuvant treatments following surgery were not included in this analysis.
That makes this study one of the uncommon studies that really tries to look at what happens when women refuse all standard therapy for breast cancer. Regular readers will remember that I’ve written about the “breast cancer alternative cure testimonial” for a long time; indeed, one of my very first posts for this blog was on just that topic. What’s important to remember about these testimonials is that, in almost all cases, the woman will have undergone some sort of potentially curative surgery, usually a lumpectomy or an excisional biopsy large enough to qualify as a lumpectomy, and then have refused further therapy; i.e., adjuvant chemotherapy, antiestrogen therapy (such as Tamoxifen), and/or radiation therapy. Adjuvant therapy is just that; it’s an adjuvant to the main treatment, which is surgery. As I’ve pointed out so many times, surgery is the main curative therapy for breast cancer for stage I and II breast cancer; the adjuvant chemotherapy and radiation therapy are just “icing on the cake,” so to speak. Radiation therapy decreases the chance that the cancer will recur in the local area in the breast where it was cut out, while chemotherapy and hormonal therapy decrease the chance that it will recur elsewhere in the body and kill the patient. (That’s a simplistic description, because there is good evidence that radiation therapy also contributes to a survival benefit, but it is, roughly speaking, a good way to articulate the benefits of adjuvant chemotherapy and radiation therapy.) In stage III breast cancer, surgery, radiation, and chemotherapy are usually all required to effect a cure, but surgery can in some cases still cure such a woman; the odds are considerably lower. It’s also important to remember that, before there was chemotherapy and radiation, surgery was the only modality that could cure breast cancer. William Halsted himself (the surgeon who developed the radical mastectomy) cured some women 120 years ago with nothing more than radical surgery.
What you will find in most breast cancer testimonials for alt-med “cures” is a woman refusing chemotherapy, hormonal therapy, and/or radiation therapy and then crediting her survival to whatever quackery she decided to try instead, when in reality it was the surgery that cured her. (Peter Moran also noted this and explained it well.) All she accomplishes by refusing additional therapy is to increase the odds that her tumor will return, but, given that in early stage cancer surgery alone has a pretty high cure rate, the woman’s odds were pretty good before receiving any chemotherapy. So right away, that makes this study important. At 185 patients, it’s one of the larger series looking at the outcomes of patients who refuse all conventional therapy. The authors used a matched analysis to pick a control group by picking matched patients who underwent conventional therapy who matched the following characteristics of the patients refusing therapy: age (± 3 years), calendar year and clinical stage at diagnosis. This control group consisted of five controls for every patient refusing therapy.
The authors then excluded patients over 75 because that has been the cutoff for clinical studies and active treatment protocols with chemotherapy in the past. This is actually one of the weaknesses of the study. Although it wasn’t all that long ago that we didn’t consider chemotherapy for women over 70, such is no longer the case. These days 75 years old no longer represents a cutoff above which chemotherapy won’t be administered. Even 80 years old is not a hard cutoff. I’ve seen our tumor board recommend chemotherapy on occasion for patients on occasion who were well into their 80s. If a patient is reasonably healthy and has a good performance status, oncologists are now increasingly willing to administer chemotherapy to much older people. However, this is a relatively recent development, and surgery has never traditionally been withheld from these elderly patients unless they are in really poor health with a life expectancy that is less than a couple of years. It’s also had not to note that the pendulum appears to be swinging back the other way, just not for older women but for all women. In other words, with the development of tests like the OncoType DX, we are getting better at figuring out who will and won’t benefit from chemotherapy at all ages. Still, given that the time period encompassed by this study is large, it was probably reasonable to make this exclusion, because in the earlier parts of the study it was probably rare for a woman over 75 to receive chemotherapy.
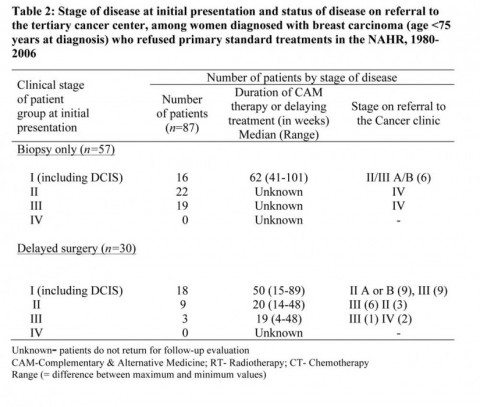
Be that as it may, that exclusion criteria left 87 patients under 75 who initially refused all therapy. The majority of patients who refused therapy were married (51%), older than 50 (61%), and urban residents (66%). As far as diagnostic criteria went, 57 patients had biopsy confirmation of their tumor only, while 30 ultimately underwent delayed surgery. 50 patients decided to undergo alternative medicine treatment, while the reasons the other 37 refused therapy were unclear or not described. The characteristics of the patients arelisted below:
It should be noted that the average delay of surgery in the patients who ultimately underwent surgery was between 20 and 30 weeks, while the delay among women who presented with stage I disease (or stage 0 disease, otherwise known as ductal carcinoma in situ) ranged from 41 to 101 weeks, with a median delay of 62 weeks. All the stage II and III patients returned to the cancer center with Stage IV disease, while the stage I patients returned with stage II, III, or IV disease. To put it more bluntly, nearly every patient who initially refused treatment progressed to a higher stage. In only four patients did the cancer fail to progress, and in none of them did the tumor shrink and downstage. It’s even uglier when we look at survival. The following graph compares disease-specific survival between patients who refused therapy and those who did not:
The difference in survival between those who underwent standard therapy shortly after thye were diagnosed with breast cancer and those who refused. The results are summarized thusly:
The 5-year overall survival was 43.2% (95% CI: 32.0 to 54.4%) for those who refused standard treatments and 81.9% (95% CI: 76.9 to 86.9%) for those who received them. The corresponding values for the disease-specific survival were 46.2% (95% CI: 34.9 to 57.6%) vs. 84.7% (95% CI: 80.0 to 89.4%).
Differences this huge are seldom seen in survival curves. Going back a ways to an older discussion of mine, in which as part of the discussion I discussed a classic paper by Bloom and Richardson that looked at the natural history of untreated breast cancer from the late 1800s to the early 1900s. The graph looks like this:
A proponent of so-called “complementary and alternative medicine” (CAM) might look at this curve and ask why the five-year survival for untreated breast cancer was around 18% while in the current study it was 43%? Aha! they might say, CAM does something! Well, not really. First, remember that 30 of the patients in the current series did ultimately undergo surgical therapy, just delayed by many weeks to several months. More importantly, remember that 100 years ago there was no mammography or ultrasound. Each and every cancer diagnosed was diagnosed when the woman had symptoms, the vast majority of a time a lump in the breast. Nearly all women were stage II or III when diagnosed. In fact, we have no idea of how many of those women already had metastatic disease at the time they were diagnosed. After all, there were no CT scanners, bone scans, or, in the early part of the time period covered by the Bloom and Richardson study, even chest X-rays. In marked contrast, far more patients from 1980 to 2006 were diagnosed by mammography, which led to a larger number of stage I cancers and especially noninvasive cancers (i.e., DCIS), which take longer to kill because they are earlier in their progression.
In brief, we’re comparing two different time periods, and we have no idea what the distribution of tumor characteristics were in the Bloom & Richardson paper compared to the characteristics of the patients in the current series. In other words, it’s just not possible to compare the two series, and, even in the absence of treatment (which includes the use of CAM, in my book), you can’t compare the series. Either way, by today’s standards, a five year median survival of 43% for all comers in breast cancer is pathetic. It probably is close to the expected five year survival in essentially untreated cases of early stage breast cancer over the last 20 years. Fortunately, we have no way of knowing for sure, as doing so would involve observing untreated women and measuring their median survival.
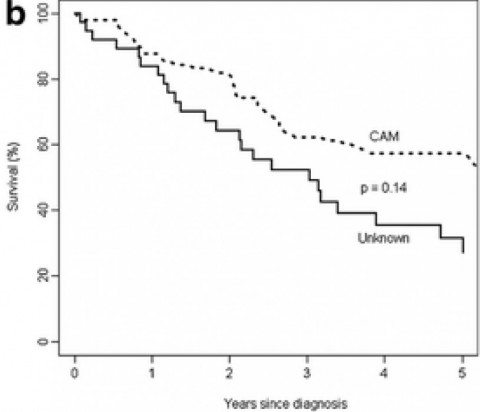
But wait! Let’s look at one more graph. This is a comparison of five year, disease-specific survival between women who chose to undergo CAM therapies instead of effective therapy and women whose reason for refusing therapy is unknown:
The authors write:
Since 58% of patients received different kinds of CAM, a comparison of the outcome was performed between groups who received CAM and those whose treatment details were not known. Figure 2 compares the survival patterns of women who refused treatment who either received CAM or for whom the reason for refusal was unknown. The 5-year overall survival was 57.4% (95% CI: 42.7 to 72.1%) for women who received CAM and 26.3% (95% CI: 11.3 to 41.3%) for those whose treatment details were unknown. The global survival for the CAM group was better than for women whose reason for refusal was unknown (p ≤ 0.05), and disease-specific survival for the CAM was better for women whose reason for refusal was unknown, but this was not statistically significant (31.5%; 95% CI: 15.1 to 48.0%).
I could see CAM supporters grasping at this graph to argue that CAM has an effect on survival. That would be grasping indeed. First, the difference in breast cancer-specific survival is not statistically significant, although the difference in overall survival is. Second, we have no idea what the distribution of stages and other relevant tumor characteristics is. Are they well matched? Probably not, but we have no idea. We also need to remember that the “unknown” group is just that, unknown. We don’t know why these patients refused therapy, and we don’t know whether or not some of them underwent some form or other of CAM treatment. In other words, more than likely the two groups were not matched for some characteristic or other. Did some of the patients who refused all therapy do so because they were at a more advanced stage and, instead of trying alternative therapy, had decided to give up? We don’t know. Were the patients who refused all therapy older? Were they sicker and therefore more afraid of undergoing therapy? We don’t know.
No matter how anyone tries to spin it, this study adds to the slowly growing body of evidence that, taken as a whole, conclusively demonstrates that (1) “conventional” science-based care works for breast cancer and (2) eschewing “conventional” science-based care has the potential to have disastrous consequences. I always tell patients after they’re first diagnosed that if there’s one “good” thing about breast cancer it’s that it’s not an emergency. There is time to think about therapeutic options and decide upon a treatment plan. The tumor has, after all, been there many months to many years, and, from a strictly biological standpoint, a delay of a month or two in treatment almost never makes much of a difference in outcomes. However, longer delays are dangerous, with the danger increasing along with the length of the delay. Choosing CAM or, let’s call it what most of it is, quackery, serves no purpose but to delay effective treatment, increase the likelihood that the cancer will progress to become incurable, and decrease the likelihood of cure. That progression can be horrible, too. Just go back and look at the case of Michaela Jakubczyk-Eckert. Do not click on the link, however, if you have a weak stomach.
At best, choosing CAM over effective therapy can preclude less invasive therapy and necessitate more radical treatments after the tumor has progressed, forcing a mastectomy when lumpectomy would have done if the tumor had been treated in a reasonable amount of time. At the worst, it can allow sufficient time for the tumor to metastasize and progress to stage IV. Choosing CAM over effective medicine not only increases the chance of dying from breast cancer, but it increases the chance of dying horribly from cancer. Suffering from carcinoma en cuirasse is a horrible, horrible way to die, and certainly refusing surgery increases the risk of carcinoma en cuirasse just as much as refusing chemotherapy increases the risk of dying of metastatic disease. This study is just another piece of evidence that reminds us of this.