Preface: On issues such as this, I think it’s always good for me to emphasize my disclaimer, in particular:
Dr. Gorski must emphasize that the opinions expressed in his posts on Science-Based Medicine are his and his alone and that all writing for this blog is done on his own time and not in any capacity representing his place of employment. His views do not represent the opinions of his department, university, hospital, or cancer institute and should never be construed as such. Finally, his writings are meant as commentary only and are therefore not meant to be used as specific health care recommendations for individuals. Readers should consult their physicians for advice regarding specific health problems or issues that they might have.
Now, on to the post…
“Early detection saves lives.”
Remember how I started a post a year and a half ago starting out with just this statement? I did it because that is the default assumption and has been so for quite a while. It’s an eminently reasonable-sounding concept that just makes sense. As I pointed out a year and a half ago, though, the question of the benefits of the early detection of cancer is more complicated than you think. Indeed, I’ve written several posts since then on the topic of mammography and breast cancer, the most recent of which I posted a mere two weeks ago. As studies have been released and my thinking on screening for breast cancer has evolved, regular readers have had a front row seat. Through it all, I hope I’ve managed to convey some of the issues involved in screening for cancer and just how difficult they are. How to screen for breast cancer, at what age to begin screening, and how to balance the benefits, risks, and costs are controversial issues, and that controversy has bubbled up to the surface into the mainstream media and public consciousness over the last year or so.
This week, all I can say is, “Here we go again”; that is, between downing slugs of ibuprofen for the headaches some controversial new guidelines for breast cancer screening are causing many of us in the cancer field.
On Monday evening, the United States Preventative Services Task Force (USPSTF) released new recommendations for screening mammography, which it published in the Annals of Internal Medicine, that have, let me tell you, shaken my specialty to the core. I must admit I was surprised at the recommendations. No, I wasn’t surprised that recommendations to change the ages and intervals recommended for mammographic screening were released. I saw something like this coming based on a series of studies, some of which I’ve discussed right here on this very blog, such as a study suggesting that one in three mammographically detected breast cancers are overdiagnosed and that as many as one in five breast cancers may spontaneously regress, coupled with evaluations suggesting that the number of lives saved by mammography is not as great as previously thought, such as this Cochrane Review updated last year. What surprised me is how much of a departure from current mammography guidelines the USPSTF recommendations were and, even more so, that they were released this year. I hadn’t expected recommendations like this this soon. But I have to deal with them, and in doing so I might as well try to help SBM readers understand them too.
The first thing that women need to understand is that these recommendations are for asymptomatic women at average risk for breast cancer undergoing routine screening for breast cancer. They are most assuredly not for women judged to be at high risk due to genetic mutations, strong family history, or other factors resulting in an elevated risk for breast cancer. Neither are these guidelines for women who are not completely asymptomatic. If you’re a woman, particularly if you’re over 40 but not limited to women over 40, and have felt a lump, that lump needs to be evaluated by a physician. Period. Screening by definition is administering a test to an asymptomatic population. These recommendations should not be used as a reason to delay or forego the evaluation of masses or other breast abnormalities. I mention this point ad nauseam because I sometimes see confusion between screening and diagnostic mammography in discussions of this issue. Again, screening mammography is for asymptomatic women. Diagnostic mammography is for women with a lump or who have been found to have abnormalities on a screening examination.
The second thing that needs to be understood is that these recommendations do not usurp the current standard of care, although it may seem that way from how they have been portrayed in the press. The American Cancer Society and other cancer organizations have not adopted them. That being said, I do rather suspect that the USPSTF guidelines are the first shot in a battle that is likely to change how we screen for mammography. How much our guidelines will change, I doubt that we will know for quite some time. That always leaves the question of what to do in the meantime. For me, that is to adhere with the current standard of care, albeit with perhaps a bit more flexibility for younger women.
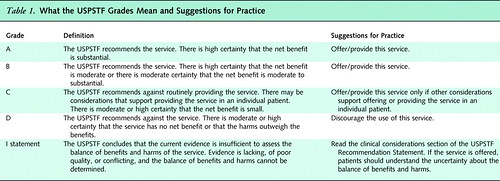
First, the discussion to follow will make a lot more sense if I mention right now that the USPSTF grades its levels of evidence using this grading scale:
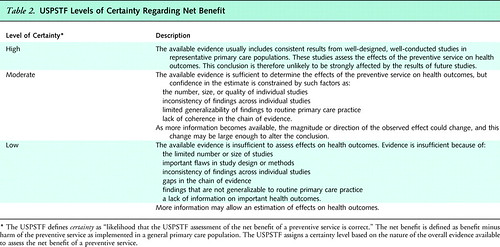
And ranks its level of certainty using this scale:
And here are its recommendations summarized:
- The USPSTF recommends against routine screening mammography in women aged 40 to 49 years. The decision to start regular, biennial screening mammography before the age of 50 years should be an individual one and take patient context into account, including the patient’s values regarding specific benefits and harms. (Grade: C recommendation.)
- The USPSTF recommends biennial screening mammography for women aged 50 to 74 years. (Grade: B recommendation.)
- The USPSTF concludes that the current evidence is insufficient to assess the additional benefits and harms of screening mammography in women 75 years or older. (Grade: I Statement.)
- The USPSTF recommends against teaching breast self-examination (BSE). (Grade: D recommendation.)
- The USPSTF concludes that the current evidence is insufficient to assess the additional benefits and harms of clinical breast examination (CBE) beyond screening mammography in women 40 years or older. (Grade: I Statement.)
- The USPSTF concludes that the current evidence is insufficient to assess the additional benefits and harms of either digital mammography or magnetic resonance imaging (MRI) instead of film mammography as screening modalities for breast cancer. (Grade: I Statement.)
And the summary for patients states:
The USPSTF found fair evidence that women who have screening mammography die of breast cancer less frequently than women who do not have it, but the benefits minus harms are small for women aged 40 to 49 years. Benefits increase as women age and their risk for breast cancer increases. However, there are relatively few studies of mammography for women aged 75 years or older. The potential harms of mammography include anxiety, procedures, and costs due to false-positive results and receiving a diagnosis and treatment of cancer that never would have surfaced on its own within a woman’s natural life time. They found that the benefit of mammography every 2 years is nearly the same as that of doing it every year, but the harms are likely to be half as common. They found no evidence that self- or clinical examination reduces breast cancer death rates.
There are two bombshells here. The first is the recommendation against routine screening mammography in women between 40 and 49. That’s the change that’s caused all sorts of controversy. Almost as big a bombshell is the recommendation for screening every other year, rather than every year. Add these two together, and it’s a recipe for confusion and controversy among women. After all, we’ve been recommending for a long time that women undergo mammography beginning at age 40 and then every year thereafter, no ifs, ands, or buts. It was a simple message, easy to transmit to women, easy to understand, simple to promote, although I would point out that it was anything but easy to convince women to undergo regular screening. Fear that it will be harder to persuade women to undergo screening may well be part of the nearly universally negative reaction to the recommendation that I’ve seen thus far from advocacy groups such as the Susan J. Komen Foundation and the American Cancer Society. I can understand how these new recommendations could be profoundly confusing to women.
That’s why it’s important to understand on what evidence these recommendations are based. It might help if you go back and read a post I wrote a couple of weeks ago that discusses a review of the literature that urged a rethinking of screening mammography. In that article, it was estimated that, for women between the ages of 50 and 70, 838 women have to be screened for over 5,866 screening visits to sayve one life. It often shocks people to hear these sorts of numbers, but they are not beyond the pale for screening programs. More importantly, the USPSTF based its update of its 2002 recommendations on newer studies, including a study included in the same issue of the Annals of Internal Medicine that used several models to estimate breast cancer risk reduction using various screening paradigms, as well as newer randomized clinical trials, such as the Age Study and updated Gothenberg trial data. These models and results are consistent with randomized clinical trial results that indicate that there is a reduction in breast cancer mortality that results from beginning screening at 40 years but the reduction is “modest and less certain than mortality reductions observed from screening women aged 50 to 69 years.” By using data from randomized clinical trials, the USPSTF estimates that averting 1 death from breast cancer requires screening 1,904 women aged 40 to 49 years; 1,339 women aged 50 to 59 years; or 377 women aged 60 to 69 years. As described above, there was little difference in the benefits between screening every year versus screening every other year, but there were considerably more harms.
The USPSTF’s recommendation not to teach breast self-examination (BSE) is another point of controversy. Despite a lot of enthusiasm for the practice, Cochrane Reviews and other evidence have failed to find convincing evidence that routine regular BSE saves lives. I wish it were otherwise, but it appears not to be, even though there are compelling anecdotes out there of women who did find a lump on BSE and it turned out to be cancer. Unfortunately, overall, the evidence to support BSE is weak. On the other hand, even the Cochrane Collaboration, which I have in the past sometimes accused of methodolatry and “nihilism” with respect to screening concluded:
Some women will continue with breast self-examination or will wish to be taught the technique. We suggest that the lack of supporting evidence from the two major studies should be discussed with these women to enable them to make an informed decision. Women should, however, be aware of any breast changes. It is possible that increased breast awareness may have contributed to the decrease in mortality from breast cancer that has been noted in some countries. Women should, therefore, be encouraged to seek medical advice if they detect any change in their breasts that may be breast cancer.
Indeed, on a purely practical level, I see nothing wrong with women being taught to be aware of how their breasts normally feel and to bring to a physician’s attention any changes that concern them and still encourage that.
So what are the harms of screening? First, there are “unnecessary” biopsies. I used quotation marks because we don’t know that the biopsies were unnecessary except in retrospect because our imaging technology is not good enough to differentiate benign from malignant as well as we would like, with as many as 80% of biopsies being negative. Second, as I’ve discussed before, there is a significant rate of overdiagnosis. Overdiagnosis is the detection of tumors that would never lead to life-threatening disease over the lifetime of the woman. Overdiagnosis leads to overtreatment because, again, we can’t identify which of these diagnosed tumors will and won’t progress; so we have to treat them all. The question then becomes: What is the risk-benefit ratio of screening. For ages 40-49, the analysis of the results by the USPSTF showed a 15% reduction in breast cancer mortality, which was similar to the risk reduction for women aged 50-59 while the risk reduction was 32% for women aged 60-69 However, given the lower incidence of breast cancer in the younger age range and the higher chance of false positives and overdiagnosis, the absolute number of lives saved is much smaller and comes at a higher cost.
But enough of all these numbers. For one thing, the supporting articles in the Annals of Internal Medicine are rather poorly written (no doubt written by a committee) and make it hard to tease out the clear comparisons of the numbers of women potentially harmed. Rather, what I want to emphasize here is that these new recommendations are a classic example of what happens when the shades of gray that characterize the messy, difficult world of clinical research meet public health policy, where simple messages are needed in order to motivate public acceptance of a screening test. It’s also an example where reasonable researchers and physicians can look at exactly the same evidence for and against screening at different ages and come to different conclusions based on a balancing of the potential benefit versus the cost and potential harms. The USPSTF simply came down on a side more like how many European nations screen for breast cancer. How this all will play out is an open question, because how breast cancer screening ultimately evolves will depend upon how women undergoing screening and we as a society end up deciding how to balance the risks and benefits of screening. It will also be affected by advances in technology and our understanding of the biology of breast cancer. The only prediction I can make is that the standard of care for breast cancer screening will almost certainly change. I doubt it will change all the way to the USPSTF’s new guidelines, but likely it will move in that direction, although I cannot predict how far. In any case, it’s always messy when that happens and leads to blowback. For instance, a professional society to which I belong issued a highly embarrassing press release, a case study in the wrong way to respond to a new set of recommendations like those of the USPSTF. The worst part of this press release was this:
We believe these recommendations effectively turn back the clock to pre-mammography days by making the diagnosis of breast cancer occur only when the tumor is large enough to be felt on a physical exam. The Society will continue to advocate for routine annual mammography screening for all women beginning at age 40. Mammography screening reduces breast cancer mortality and saves lives.
By this standard, I suppose much of Europe is “pre-mammography,” given that many countries in Europe use guidelines for screening mammography very much like what the USPSTF recommended. Nothing in the guidelines even suggests going back to those days. Reasonable physicians and scientists can disagree over whether the new guidelines represent a defensible attempt to apply current evidence about screening mammography to public health policy, but demonizing the USPSTF’s recommendations with such inflammatory language is neither productive nor reasonable. If you’re going to argue against the new guidelines, at least try to argue the evidence and counter what the guidelines actually say, as the American Cancer Society did:
- The USPSTF says that screening 1,339 women in their 50s to save one life makes screening worthwhile in that age group. Yet USPSTF also says screening 1,904 women ages 40 to 49 in order to save one life is not worthwhile. The American Cancer Society feels that in both cases, the lifesaving benefits of screening outweigh any potential harms. Surveys of women show that they are aware of these limitations, and also place high value on detecting breast cancer early.
- With its new recommendations, the USPSTF is essentially telling women that mammography at age 40 to 49 saves lives; just not enough of them. The task force says screening women in their 40s would reduce their risk of death from breast cancer by 15 percent, just as it does for women in their 50s. But because women in their 40s are at lower risk of the disease than women 50 and above, the USPSTF says the actual number of lives saved is not enough to recommend widespread screening. The most recent data show us that approximately 17 percent of breast cancer deaths occurred in women who were diagnosed in their 40s, and 22 percent occurred in women diagnosed in their 50s. Breast cancer is a serious health problem facing adult women, and mammography is part of our solution beginning at age 40 for average risk women.
This is a far more reasonable and nuanced critique that encapsulates starkly what the issues are. In essence, the ACS agrees with the conclusions of the data used by the USPSTF to support its recommendations but disagrees with the value judgments behind its recommendations to back off on screening in women under 50 and to decrease screening frequency to every other year. However, even the ACS couldn’t resist a little holding back in that it didn’t mention the raw numbers of lives potentially saved in each age group. In any case, I think the response from the American Society of Clinical Oncology (ASCO, a society to which I also belong) was much better. It did what I support, namely defending the availability of mammography to women over 40, while suggesting a more personalized approach to screening that represents a reasonable compromise between current screening recommendations that encompasses what the USPSTF has recommended:
Today’s recommendations from the USPSTF recognize the value of mammography in reducing breast cancer deaths, affirm the importance of mammography among women aged 50 and older, and emphasize that mammography should be seriously considered in women 40 to 49 after assessment of the risks and benefits. It is therefore of concern that at present more than a third of women who are now recommended for screening are not getting regular mammograms. While the optimal scheduling of regular mammograms is being discussed by experts in the field, ASCO would not want to see any impediments to mammography screening for any woman age 40 and above.
From ASCO’s perspective, the critical message is that all women – beginning at age 40 — should speak with their doctors about mammography to understand the benefits and potential risks, and determine what is best for them.
And that’s what it’s really about. The patient and her physician collaboratively determining what is best for her. Indeed, the current recommendations of the USPSTF are no less arbitrarythan previous recommendations for screening. What they reflect are newer studies and a different analysis of the the risk-benefit ratio, in which the more modest benefits of routine mammography in women between ages 40-49 at average risk for breast cancer are judged not to be worth the potential harm caused. Others may look at the same data and decide that the benefits of screening mammography in this age range are worth the potential harms. Individual women may hear the same benefits and risks and decide differently for themselves. Neither view is clearly inherently “right” or “wrong,” and what I hope we should all be able to agree upon is that women should be aware of and understand as much as possible those tradeoffs regardless before deciding upon screening.
In the meantime, I’m not quite buying that these new recommendations are so clearly more “science-based” than the older recommendations when, as the ACS points out, the USPSTF arbitrarily decided that screening 1,300 women to save one life is an acceptable cost but screening 1,900 to save a life is not. I do, however, think that we health care professionals have probably not sufficiently described the potential harms that come from screening in the past, and the controversy surrounding these guidelines is that failure coming home to roost. As I’ve written before, I sincerely hope that better technology and the discovery of new biomarkers can decrease these high numbers by increasing the specificity of mammographic screening and, possibly, even allowing us to identify which mammographically detected tumors don’t need treatment. Indeed, to me, the one advance that could most reduce the potential for overtreatment of image-detected breast cancer would be molecular tests that would accurately allow us to identify accurately the subset of breast cancers that are unlikely ever to progress and threaten the life of the woman. Another advance would be better imaging technology that could more accurately distinguish cancer from non-cancer or achieve the same thing as mammography without compression or radiation, which could lead to greater acceptance of screening. Finally, better biomarkers and tests that allow us to assess more accurately a woman’s true risk of developing breast cancer would permit targeted recommendations tailored to a woman’s individual risk. All of these are being actively researched, some at my own institution, but until such technologies and tests are developed we are left with mammography. As imperfect as it is, it is the best screening tool we currently have.
In the meantime, the application of science-based medicine to screening asymptomatic people for disease cannot avoid becoming interwined with a parallel discussion of how to balance risks and benefits, as well as a discussion of values. In the case of breast cancer, starting at 40 appears only to modestly decrease the absolute number of lives lost from breast cancer but at a fairly high cost of overdiagnosis and overtreatment, while screening yearly only increases the detection of breast cancer marginally compared to screening every year, also at a high cost in terms of more biopsies and more overdiagnosis. Whether the cost is judged to be worth it or not has to be evaluated on two levels. First and foremost, what matters is the woman being screened, what she values, and what her tolerance is for paying the price of screening at an earlier age, such as a high risk for overdiagnosis, excessive biopsies, and overtreatment in order to detect cancer earlier versus a relatively low probability of avoiding death from breast cancer as a result of undergoing regular screening. The next level is the public health policy level, where we as a society have to decide what tradeoffs we’re willing to make to save a life that otherwise would have been lost to breast cancer. Although screening programs and recommendations should be based on the best science we currently have, deciding upon the actual cutoffs regarding who is and is not going to be recommended to undergo screening and how often women should be screened unavoidably involves value judgments by those being screened, physicians recommending screening, and society at large.
It is just those value judgments that are driving the debate spawned by the USPSTF recommendations, a debate that is too frequently acrimonious when it doesn’t have to be.