
How do you like your coffee? Rectally?
Fill it to the rim? Please don't.

How To Respond to Anti-Vaxxers
How do we best address the anti-vaccine phenomenon? It's complicated.

Pseudoscience in Child and Adolescent Psychotherapy
This new book addresses the neglected field of research on child and adolescent psychotherapy and does an excellent job of distinguishing treatments that have been proven to work from treatments that are based on pseudoscience.

The Paddison Program for rheumatoid arthritis: An unproven treatment that provides only the illusion of control
Clint Paddison is an Australian comedian with a science degree who developed rheumatoid arthritis at age 31. He now claims to have controlled it with a diet he developed to alter the gut microbiome. How plausible is his story, and does his Paddison Program work? Answer: Not very and almost certainly no.

Maine considers protecting quacks from accountability to regulators and patients
The Maine Legislature is considering a bill that would put quacks beyond the reach of state healthcare regulatory authorities and leave patients without effective redress for harms.

JAMA on Medical Misinformation
A JAMA article addresses the issue of confronting medical misinformation. They make good recommendations - but do not go nearly far enough.
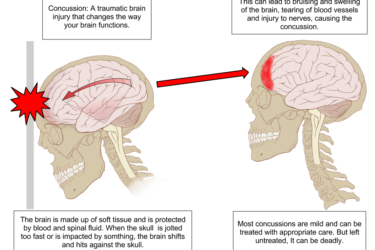
Chiropractor Treating Concussions for Earlier Return to Play
A chiropractor is using questionable diagnostic and therapeutic measures to return athletes to play sooner after a concussion. Not a good idea.

Bleaching away what ails you: The Genesis II Church is still selling Miracle Mineral Supplement as a cure-all
Miracle Mineral Supplement (MMS) has been sold by the Genesis II Church of Health and Healing as a cure-all to treat conditions and diseases as diverse as autism, cancer, diabetes, multiple sclerosis, and malaria. Indeed, it's touted as a cure for nearly all disease. It is, however, basically industrial bleach. As ridiculous and harmful as MMS is, it's a quackery that just...

New Research Reveals a Startling Increase in Pediatric Foreign-Body Ingestions
New research has revealed a significant increase in pediatric foreign-body ingestions over the past 20 years, including life-threatening batteries and magnets.







Don’t Blame the Patient