
The So-Called Vaccine Debate: False Balance in The San Diego Union-Tribune
A recent article in The San Diego Union-Tribune presents a pair of articles that gives a false balance regarding vaccinations. Those who oppose vaccination do so on the basis of ideology rather than science, thus placing the public's health at risk.

The Six Month Dental Recall – Science or Legend?
The evidence to support dental cleaning every six months is...less than ideal, but it still may be a good idea for many people.

Are we all contaminated with chemical toxins?
Are we all being gradually poisoned by environmental toxins? And what is the evidence for detoxification kits and cleanses?
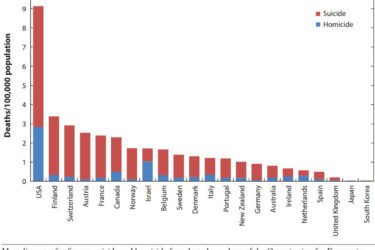
Gun Violence as a Public Health Issue
Gun violence is a serious public health issue in America but is not getting the research that it deserves. This needs to change.

A Cornucopia of Crislip
Mark Crislip has written three books. They are full of wisdom, science-based thinking, and hilarious humor. Highly recommended.

True believers, entrepreneurs, and scammers in alternative medicine
In the online echo chamber promoting alternative medicine, there are varying degrees of deception. There are true believers (who are often victims), entrepreneurs (who are often true believers who found a profitable business), and scammers. The categories are not mutually exclusive.
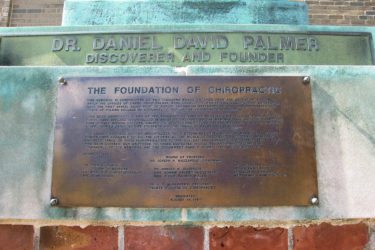
Inside Chiropractic: Yesteryear and Today
In the 123 years since its inception, the core beliefs of the chiropractic profession have not changed. Chiropractic continues to exist as a form of alternative medicine that embraces a variety of questionable procedures and treatment methods. The chiropractic profession in the United States is still defined by the vertebral subluxation theory that gave it birth and independence as an alternative to...

Cleveland Clinic genetic experts call out functional medicine on worthless genetic testing and supplement prescribing
Cleveland Clinic genetics experts call out functional medicine on worthless genetic testing and dietary supplement prescribing: "Poor science, leading to even worse medicine." Irony meters exploded everywhere.

Move
For most people, common health goals are best approached with as simple a strategy as possible. This avoids cognitive overload and non-compliance. Get the basics right, as there are diminishing returns from increasingly arcane details.

Answering Our Critics – Again!
Critics of Science-Based Medicine keep making the same old tired arguments, despite the fact that their arguments have been repeatedly demolished. Here is a list of recurrent memes, with counterarguments.






Don’t Blame the Patient