The New York Times: Promoting False Hope as Journalism
The New York Times sells a narrative of false hope, and fails to engage in even basic journalism to tell a more complete story.

Medical Neglect of Children
Medical neglect caused horrific suffering for these children, ending in death or permanent impairment. Their parents failed them, but so did society.
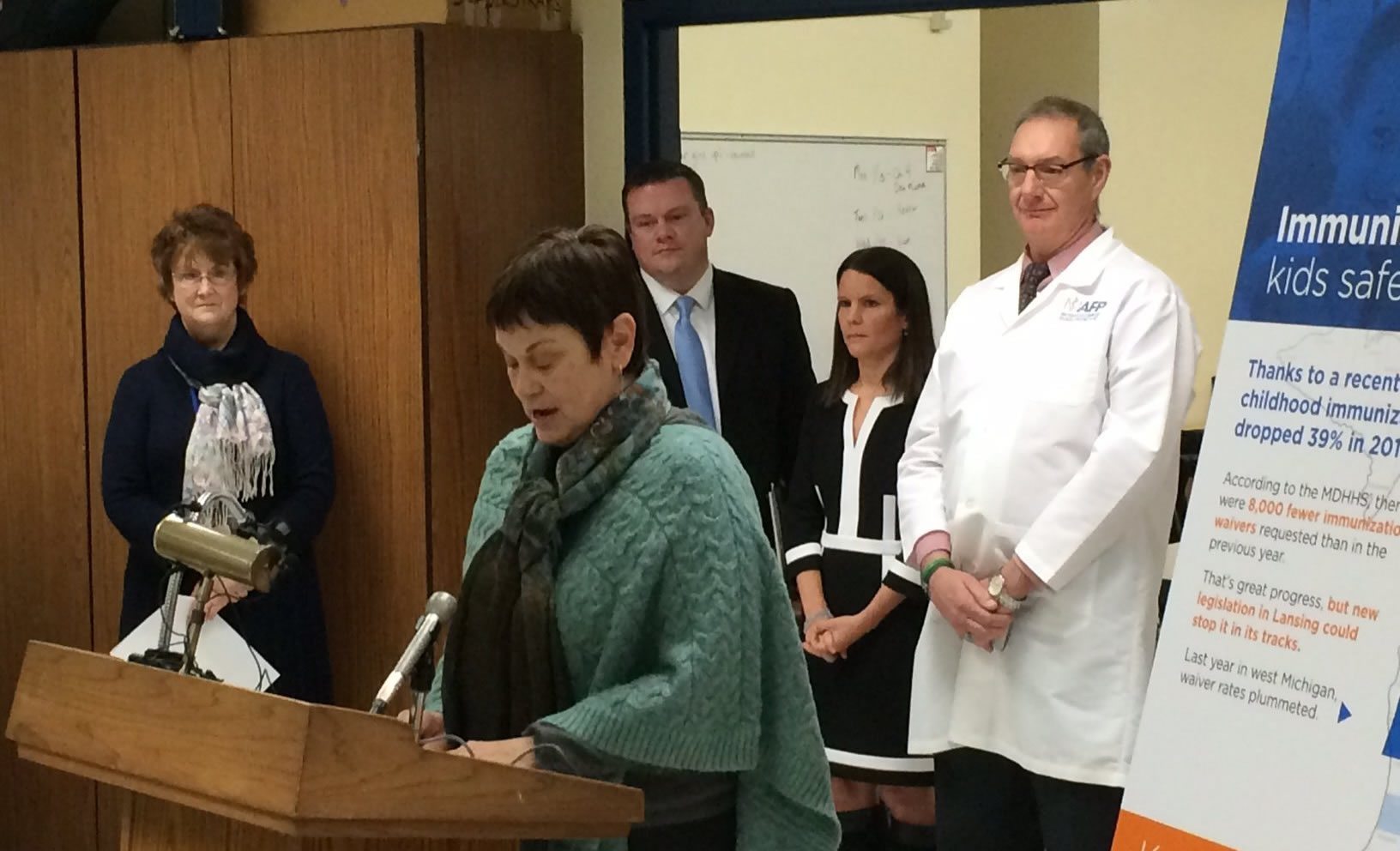
Make measles great again: A case study of the politicization of school vaccine requirements in Michigan
Protecting our children through school vaccine requirements has long had strong bipartisan support. Unfortunately, the antivaccine movement has had success linking "vaccine choice" with "freedom" and "parental rights", leading to a surge of right wing antivaccine activism that has undermined that bipartisan consensus. Two bills under consideration by the Michigan legislature represent a microcosm of what is going on in much of...
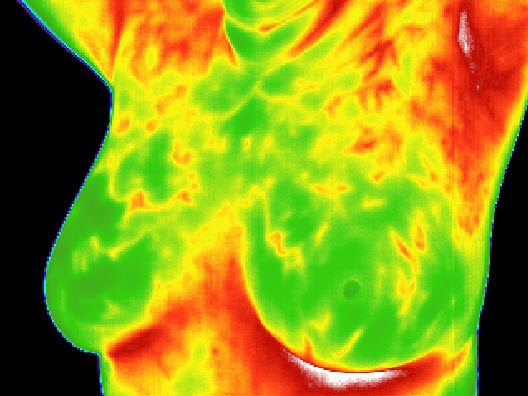
FDA issues warning letter to “holistic” practitioner offering thermography for breast cancer detection
Thermography for breast cancer detection is one of more than 65 products the FDA just announced it is going after for fraudulently claiming to prevent, diagnose, treat or cure cancer.

Outbreaks among Somali immigrants in Minnesota: Thanks for the measles again, Andy
Andrew Wakefield's antivaccine propaganda film VAXXED claims that MMR vaccination causes autism in African American boys. Unfortunately, this is not the first time Wakefield has targeted people of color with antivaccine misinformation. Before there was VAXXED, Wakefield and antivaxers targeted Somali immigrants in Minnesota. Measles outbreaks have been the result.









Faking Peer-Review
A major cancer journal just retracted 107 papers for faking peer-review, bringing the total for that publisher to 450. How did this happen, and how do we prevent it in the future?