Category: Health Fraud

The Dawning of Friends of Science in Medicine (FSM)
For over 10 years, Friends of Science in Medicine has been fighting quackery, fraud, and pseudoscience in Australia.

How we got here with political and health misinformation: The case of “Hacker X” and Mike Adams
Ars Technica recently published a story about Hacker X, who helped Mike Adams expand his online empire of health fraud into an empire of fake news and political disinformation, thus intertwining health and political misinformation into the deadly combination we see now.

Ivermectin is the new hydroxychloroquine, take 6: Incompetence and fraud everywhere!
Ivermectin is the new hydroxychloroquine, a drug repurposed for COVID-19 that almost certainly doesn't work but is still being touted as a "miracle cure" by quacks, grifters, and political ideologues. Are the data supporting it all fraud?

Olympic Pseudoscience – Tokyo Edition
Pseudosciences come and go with the Olympics.

Supreme Court rules that FTC cannot seek restitution on behalf of consumers
The U.S. Supreme Court recently ruled that the FTC lacks the authority to seek consumer refunds and other monetary relief from scammers. Without a fix from Congress, the ability of the FTC, and perhaps other agencies, to redress financial injuries caused by quacks and other frauds is greatly diminished.

“Quack Protection Acts” proposed in state legislatures
Laws protecting "complementary and alternative" health care providers from state regulation have been proposed in several state legislatures under the rubric of "health freedom". These "Quack Protection Acts" harm consumers.

The “Disinformation Dozen” spreading anti-vaccine messaging on social media
Just twelve individuals are generating two-thirds of all of the anti-vaccine messaging on Twitter and Facebook.

The Brownstein protocol is not a proven treatment for COVID-19
Dr. David Brownstein is a "holistic" physician who practices in Dr. Gorski's neck of the woods. Unfortunately, he just wrote a book promoting an unproven protocol involving vitamins, nebulized hydrogen peroxide and iodine, and intravenous ozone to treat COVID-19. There is no evidence that his protocol works, other than a very poor quality case series.
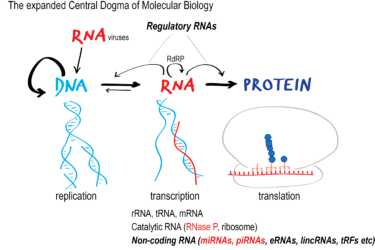
The latest antivax false claim: mRNA vaccines against COVID-19 are not vaccines but “medical devices” or “gene therapy”
There's a new antivaccine talking point in town, and it's just as much disinformation as other antivaccine talking points. It's the claim that mRNA COVID-19 vaccines are not really vaccines but "medical devices," "gene therapy," or "experimental biologics" and that they were falsely classified as vaccines in order to bypass safety testing. Here, we discuss why this claim is utter nonsense based...

COVID-19 vaccine rollout creates new scamming opportunities for crooks
As new COVID-19 vaccines become available to the public, swindlers are adjusting their cons to fit the moment, even going door-to-door to peddle their scams.

