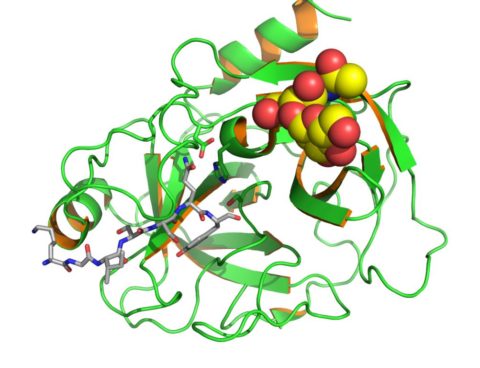
The prostate specific antigen.
You’ve all heard the dramatic testimonials in the media: “I had a PSA test and they found my prostate cancer early enough to treat it. The test saved my life. You should get tested too.” The subject of screening tests is one that confuses the public. On the surface, it would seem that if you can screen everyone and find abnormalities before they become symptomatic, only good would result. That’s not true. Screening tests do harm as well as good, and we need to carefully consider the trade-offs.
About half of American men over the age of 50 have had a PSA (prostate-specific antigen) screening test for prostate cancer. Recommendations for screening vary. The US Preventive Services Taskforce (USPSTF) says there is insufficient evidence to recommend screening. The American Urological Association and the American Cancer Society recommend screening. Urologists practice what they preach: 95% of male urologists over the age of 50 have been screened. But other groups like the American Academy of Family Physicians recommend discussing the pros and cons of screening with patients and letting them make an informed choice.
Two recent studies published simultaneously in The New England Journal of Medicine have added to the controversy. One concluded that screening does not reduce deaths from prostate cancer; the other concluded that it reduces deaths by 20%.
The PCLO Cancer Screening Trial
The Prostate, Lung, Colorectal and Ovarian (PCLO) Cancer Screening Trial involved 76,693 men in 10 US study centers. Subjects in the study group were offered annual screening with PSA for 6 years and annual digital rectal exams for 4 years; the control group received “usual care” (which could include screening – 52 percent of the control group had screening in the 6th year.) They found 2820 cancers in the screening group and 2322 cancers in the control group. There were 50 deaths in the screening group and 44 deaths in the control group, not significantly different. There was no reduction of prostate cancer mortality in 7 years of follow-up. One could argue that the effect of screening was diluted by the high rate of screening in the control group, or that longer follow-up might show a difference.
The European Randomized Study of Screening for Prostate Cancer
In the European Randomized Study of Screening for Prostate Cancer, 182,000 men age 50-74 in 7 countries were offered PSA screening every 4 years. 82% accepted at least one offer of screening. After 9 years follow-up the death rate from prostate cancer decreased by 20% but was associated with a high risk of overdiagnosis. There were 214 prostate cancer deaths in the screened group and 326 in the control group. From the statistics of those who were actually screened, one can calculate that 1068 men would need to be screened and 48 would need to be treated to prevent one death from prostate cancer. There was no reduction in all-cause mortality – what does a reduction in deaths from prostate cancer mean if there is no reduction of deaths overall? The absolute reduction in deaths from prostate cancer was 7 deaths per 10,000 men screened. 73,000 men in the screening group underwent more than 17,000 biopsies.
The downside
For any screening test, the benefits must be weighed against the risks. There are significant risks to PSA screening: biopsies, surgery, hormone treatment, chemotherapy, impotence, incontinence. Some of the men who suffer these invasive procedures and side effects would probably have lived to die of something else if they had not been diagnosed. Many prostate cancers are slow-growing and not actually life-threatening. For most of these men, it would probably have been better if they had not been screened and had never known they had prostate cancer. Screening leads to over-diagnosis, and some people get treated because of false positive tests – they never actually had the disease.
It boils down to a value judgment. Is it worth screening 1,068 men and treating 48 to save one life from prostate cancer when you don’t save lives overall? How do you weigh the costs and the suffering against the value of a life saved? There is no easy answer. Future research will try to assess things like quality of life and cost effectiveness, and we may come up with better recommendations about when to test and what level of PSA to use as a cut-off.
In an accompanying editorial in the same issue of NEJM, Michael J. Barry MD concluded:
PSA screening has at best a modest effect on prostate-cancer mortality during the first decade of follow-up. This benefit comes at the cost of substantial overdiagnosis and overtreatment. It is important to remember that the key question is not whether PSA screening is effective but whether it does more good than harm. For this reason, comparisons of the ERSPC estimates of the effectiveness of PSA screening with, for example, the similarly modest effectiveness of breast-cancer screening cannot be made without simultaneously appreciating the much higher risks of overdiagnosis and overtreatment associated with PSA screening.
