Pediatricians, particularly those who spend a significant amount of time caring for newborns, see a lot of babies with unusually-shaped heads. Although to be fair, the fact that the overwhelming majority of vaginally-delivered babies, and quite a few born via Caesarean section, will have a transient and abnormal shape to their heads makes it, well, not unusual. In fact, I rarely make it out of the room without some discussion and reassurance regarding the lumps and bumps of a new arrival’s head.
The potentially lumpy and misshapen head of the newborn occurs for a variety of reasons, some common and some extremely rare. It often is related to the development of the bones of the skull but can also involve the surrounding tissues of the scalp. A vaginal delivery, and some difficult Caesarean births, subject a baby’s head to a lot of pressure. This pressure frequently results in swelling of the scalp that can be quite impressive, but tends to resolve in a day or two.
This same pressure can also cause bleeding, perhaps because of an insufficient amount of vitamin K available to optimally activate clotting, that collects under the top layer of one or more of the bones of the skull. These cephalohematomas can also be impressive and may take weeks to completely resolve. Rarely the trapped blood becomes calcified and requires surgical correction to remove the otherwise-permanent lump and restore a normal contour to the head.
Newborns very frequently have a molded skull. Depending on the timing and severity of the pressure experienced during delivery, the shape and size of the uterus and positioning of the baby in the womb, the newborn can emerge with a variety of head shapes. The most common one that I see is a cone. If you’re thinking of a classic Saturday Night Live sketch right now, you’ve got the correct mental image.
Babies who are breech also have a distinct pattern of molding which involves a flattened and elongated top of the head because of pressure against the uterine wall. Abnormal positioning in the womb can also result in asymmetric molding of the head and facial structures like the jaw, nose and ear. Fortunately these pressure-induced and positional deformities usually resolve without intervention, often within a few days, but some are serious enough to require intervention and even surgical correction.
Why are the cranial bones of newborns so easily molded by the pressure of birth? This is a question I answer frequently for new parents and inexperienced medical students. The answer will segue us into the primary topic of this post, but before I discuss craniosynostosis, and the sadly unsurprising claims of some in the chiropractic community, a review of normal cranial anatomy is in order.
Why are newborn skulls so easily molded?
The skull of a typical healthy newborn is not just one large bone but is actually comprised of several bony plates, each joined by fibrous joints called sutures. These sutures, the major ones running mid-line down the top (sagittal) and diagonally and bilateral at the front (coronal) and back (lambdoid) of the skull, are made of strong connective tissue similar to the attachments of the teeth to the bony sockets. When fused, they allow minimal but usually clinically-insignificant movement.
But sutures in the newborn, the most well-known being the “soft spots” at the front and back of the skull, are not normally fused. The ability to shift freely with significant pressure allows for molding, so the skull doesn’t fracture or become stuck as it makes its way through the pelvis, and for the safe growth of the brain over the first two decades of life. The most rapid period of brain growth, the first two years of life, results in a brain that is four times larger than at birth. Without the ability to accommodate the expansion of the brain, a variety of problems can arise.
What is the normal pattern of cranial growth and fusion?
As the brain grows, it exerts outward pressure which pushes the bones of the skull apart. In response, new bone is formed along the edges of the cranial bones at the sutures. So appropriate growth, and this is important for later discussion of abnormal early fusion, occurs perpendicular to the suture line.
Normal fusion of the bones of the skull occurs in a reproducible pattern. At roughly two months of age, the posterior fontanel should be closed. At around two years, the anterior fontanel should no longer be palpable. The linear sutures fuse more slowly, with completion not occurring until well after full growth is achieved, but the ability of the bones to move relative to themselves to any meaningful degree is gone by two to three years of age. And prior to that it would still require significant amounts of pressure that would risk pain and injury to the skull and underlying brain.
What happens when fusion of cranial bones occurs too early?
Abnormal early fusion of one or more of the cranial sutures, known as craniosynostosis, is diagnosed in roughly 1 out of every 2000 to 2500 babies around the world. In a bit over half of cases, early fusion affects the sagittal suture that runs down the top of the head and separates the parietal bones of the skull. The second most common location is the coronal suture which runs from ear to ear separating the frontal and parietal bones.
Most of the time, craniosynostosis is an isolated abnormality with only partial fusion of one suture. But multiple sutures are prematurely fused in about 10% of cases, and this generally occurs due to a genetic syndrome with other dysmorphic features, such as cleft palate and fusion of the finger bones. Several specific gene defects resulting in craniosynostosis syndromes have been identified, typically in the fibroblast growth factor receptor family, the most well-known examples being Apert, Crouzon and Pfeiffer syndrome.
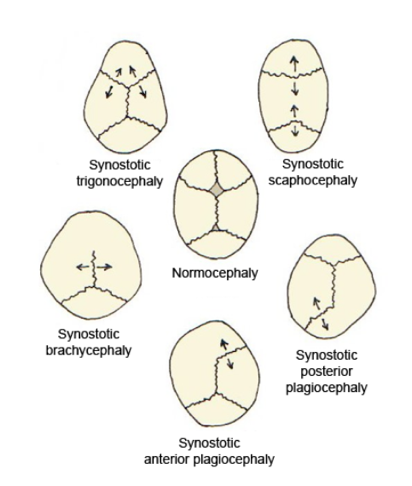
When a suture is fused too early, it restricts the growth of the skull in a predictable way. Remember earlier when I pointed out that normal growth occurs perpendicular to the suture line? If a suture is fused, normal perpendicular growth can’t occur, which accentuates growth at the sutures that aren’t fused because of increased pressure. So growth of the head will only occur parallel to the fused sutures.
For example, in the case of sagittal suture fusion the head tends to become strikingly long and narrow, a shape known as scaphocephaly. This translates to “boat skull.” When the coronal suture is fused prematurely on both sides of the forehead, the resulting shape is known as brachycephaly or “short skull.” The skull will be shortened from front to back but abnormally wide, and if untreated will begin to preferentially grow upward as well. So depending on which sutures are fused before their time, and if the fusion occurs on one or both sides of the head, there are a variety of recognized pathognomonic shapes ranging from mild to extreme.
How is craniosynostosis diagnosed and treated?
The diagnosis of abnormal early fusion of one or more sutures should be suspected when the shape of the head is abnormal. In the case of genetic syndromes, when multiple sutures are involved and associated dysmorphic features are present, it can be fairly easy to recognize. When the sagittal suture is involved, as it is in about half of cases, the classic head shape is an extremely helpful clue. But in the case of isolated non-syndromic premature fusion of other sutures, it isn’t always clear because abnormal head shape related to positioning of the infant’s head during sleep can mimic craniosynostosis.
Pediatricians see a lot of what is known as positional plagiocephaly (“twisted skull”), a phenomenon which increased significantly after universal recommendations that young infants sleep only on their backs in order to reduce the risk of SIDS. When children sleep on their backs, and especially when they have a persistent side preference, there can be significant flattening to one side of the skull. This is also more common in babies with difficulty turning the head from side to side, as occurs in a condition known as torticollis, or when they have neurological injury or disease resulting in difficulty moving at all.
It is important to consider conditions that mimic craniosynostosis because they can often be managed successfully without surgery. Positional plagiocephaly often responds to lifestyle changes, such as increased time off the back and repositioning of the head during sleep, and to physical therapy in the case of torticollis. Often suspected mild craniosynostosis resolves spontaneously before any significant diagnostic work-up is initiated. When it is severe, or doesn’t improve after a few weeks of conservative measures, the appropriate means of confirming the diagnosis is CT imaging of the skull.
Timely diagnosis and treatment of craniosynostosis is very important in order to prevent the development of complications. The most concerning potential complication is increased intracranial pressure and impaired growth of the brain. Untreated craniosynostosis can result in cognitive deficits and neurodevelopmental delays in feeding, vision, hearing and speech. It can also be a cosmetic concern that shouldn’t be taken lightly as it is linked with difficulty in social development that can have lifelong repercussions.
Except in very mild cases that are not associated with risk of increased intracranial pressure or problems with socialization, surgery is required. The complexity of management is naturally determined by the severity of the presentation and the presence of other dysmorphic features such as a cleft palate. Optimal outcomes depend on a multi-disciplinary approach that involves surgeons, pediatricians, dentists, a variety of other medical subspecialists, and various therapists. Many pediatric facilities have craniofacial teams set up for just such situations.
What does chiropractic have to do with craniosynostosis?
Unfortunately, there are practitioners of so-called complementary and alternative (or integrative) medicine out there claiming to be able to correct abnormally-shaped infant skulls. Long time readers of SBM are probably familiar with the pseudoscience known as craniosacral therapy. Drs. Hall, Crislip, and Ritchey have discussed this topic in detail in the past, although not in the setting of treating craniosynostosis. Of note, Dr. Hall links to the report of a 2-day-old child who died from injury to the brain caused by craniosacral therapy at the hands of a rogue dentist.
As I have discussed in prior posts, there are few things that chiropractors love more than a good anecdote trumped up as a case report and published in one of their low-quality journals. In fact, my first post for SBM looked at one such example of chiropractic “research” as it applies to the treatment of Tourette syndrome. Case reports when properly utilized, and their inherent weaknesses taken into account, can be a meaningful component of science-based medicine. But in the world of chiropractic they are frequently used to make inappropriate claims of treatment efficacy and as part of practice-building efforts.
One such case report exists for the use of chiropractic to correct potential craniosynostosis, the low plausibility of which rivals even homeopathy. Authored by chiropractor Joel Alcantara, the Director of Research for the International Chiropractic Pediatric Association, and published in their Journal of Pediatric, Maternal & Family Health – Chiropractic, the report discusses a 3-week-old infant supposedly diagnosed with craniosynostosis by her obstetrician and pediatrician.
The mother of the infant is described as having sought out chiropractic care during a period of recommended observation. If at that point the problem had not resolved, imaging and surgery would be arranged. The report describes the child as having a fused posterior fontanel, something that can’t be diagnosed by simple palpation, and an open but small anterior fontanel. It then describes the discovery of subluxations at multiple locations along the spine as well as the right temporomandibular joint. There were apparently also “cranial distortions of the right frontal/parietal and left parietal/occipital bones.”
The patient underwent “specific, gentle high velocity, low-amplitude type thrust” to the subluxations, as well as craniosacral therapy. After six visits, her “skull diameter” increased by roughly 5 cm from 34.5 to 39.2 cm. This is odd considering that skull diameter is not a routine measurement. I assume that they mean head circumference, which is on average 34.5 cm at birth in a term infant. If accurate, this demonstrates normal growth of the child’s head.
After her series of 13 chiropractic adjustments and “craniosacral therapy”, she was evaluated by appropriate medical professionals at almost 4 months of age who determined that surgery was not indicated. This is wonderful news of course, but it had absolutely nothing to do with subluxations or cranial distortions. From what I can piece together using the abstract, accompanying press release and some online discussion of the case by a chiropractor on her practice website, the child likely never had craniosynostosis.
Craniosynostosis is often only suspected by pediatricians. In the case of a nonsyndromic child with potential isolated early fusion, a period of observation prior to exposing them to the ionizing radiation of a CT scan can be very appropriate. These children are seen regularly to monitor for worsening of the shape of the head despite conservative measures, and signs or symptoms of increased intracranial pressure, and in many cases imaging and surgery are not needed. A false alarm is orders of magnitude more likely than chiropractic intervention reversing a fused suture, something which would require more force than pulling out a healthy tooth.
Alcantra, the author of the case report, was considerably more optimistic about the findings:
In this case we have a defect in the infant’s skull that did not require a planned surgery following a trial of chiropractic care of the spine and skull.
And:
While this is only a single case study, it shows what can happen when chiropractic to correct spinal and cranial distortions is included as a health care option for children.
In the press release, the journal’s editor Mathew McCoy also seems to conclude that the case proves efficacy:
Chiropractors work with the alignment and movement of the bones that make up the spine and many chiropractors also work on the bones of the skull, especially in children where its normal development is so crucial. So it is not so surprising that you’d see this type of outcome.
I agree that it isn’t surprising, but not that chiropractic had anything to do with it.
Unfortunately, it isn’t just that chiropractors are touting their ability to manipulate the positioning of the bones of the skull and unlock fused sutures. I easily found the blogs of clearly well-meaning but misinformed parents discussing their use of chiropractic for craniosynostosis. This post, which is found very high on Google when searching “chiropractic AND craniosynostosis” implies that it has benefit. If curious families don’t read the future posts, they won’t see that when imaging was eventually performed there was no improvement and successful surgery took place.
Conclusion
Abnormal head shape in the newborn period is extremely common and has varied causes. Premature fusion of the cranial bones, while less common, is a very serious condition that generally requires surgical correction because fused sutures are extremely strong. Improperly managed, craniosynostosis can lead to lifelong developmental delays, cognitive impairment and psychosocial difficulties.
Chiropractors who claim to be able to shift the bones of the skull, especially in children with craniosynostosis, are deluded. There is no evidence that chiropractic subluxations exist let alone play a role in the shape of the head. And it would take extreme pressure to move unfused skull bones, which would risk harming or even killing a young infant. Luckily, craniosacral therapy typically involves nothing more than a head massage and most chiropractors use gentle adjusting techniques.
Taking money from families without providing any actual benefit is wrong, but it isn’t my main concern. Abnormal head shapes do often correct on their own if related to birth pressure, which can give the appearance of chiropractic success, but many babies require true intervention. Education on proper positioning, physical therapy and even fitted helmets are common non-surgical treatments. If parents are delaying science-based medical care, it risks poor cosmetic and psychosocial outcomes. And if a child has actual craniosynostosis, improper management can also be dangerous.

