Tag: cancer

ASCO endorses the integration of quackery into breast cancer care
In 2014, the Society for Integrative Oncology first published clinical guidelines for the care of breast cancer patients. Not surprisingly, SIO advocated "integrating" dubious therapies with oncology. Last week, the most influential oncology society, the American Society of Clinical Oncology (ASCO), endorsed a 2017 update to the SIO guidelines, thus endorsing the "integration" of quackery with oncology and paving the way for...

Another pebble in the quackademic integrative avalanche
We've documented the infiltration of quackery into academic medicine through the "integration" of mystical and prescientific treatment modalities into medicine. Here, we look at a pebble in the quackademic avalanche. Is it too late for the pebbles to vote?

The Nation indulges in fear mongering about cell phones and cancer
An article published last week in the Nation likens wireless telephone companies to tobacco and fossil fuel episodes in their tactics of spreading fear, misinformation, and doubt regarding the science of cell phone radiation and health. To produce this narrative, the investigation's authors rely on unreliable sources and cherry pick scientific studies, ignoring the scientific consensus that cell phone radiation almost certainly...

The deadly false hope of German alternative cancer clinics
We at SBM have written about German cancer clinics that offer a combination of cancer quackery, some real medicine, plus unproven experimental therapies, all at a high cost, both financially and in false hope. Finally, an exposé of these clinics has been published. What these clinics are doing is even worse than even we had feared.

Snake-Based Medicine? Another Salmonella Infection Linked to Rattlesnake Pills
Rattlesnake pills, another entry in a long line of bogus cancer cures, have been linked (again) to a potentially deadly Salmonella infection.

Why do some women refuse treatments for their breast cancer?
Adjuvant therapy after surgery, such as chemotherapy, hormonal therapy, and radiation therapy, has contributed to a 39% decrease in breast cancer mortality since 1989. Unfortunately, a significant number of women decline evidence-based adjuvant therapy. A recent study suggests that distrust of the medical system plays a significant role in such refusal.
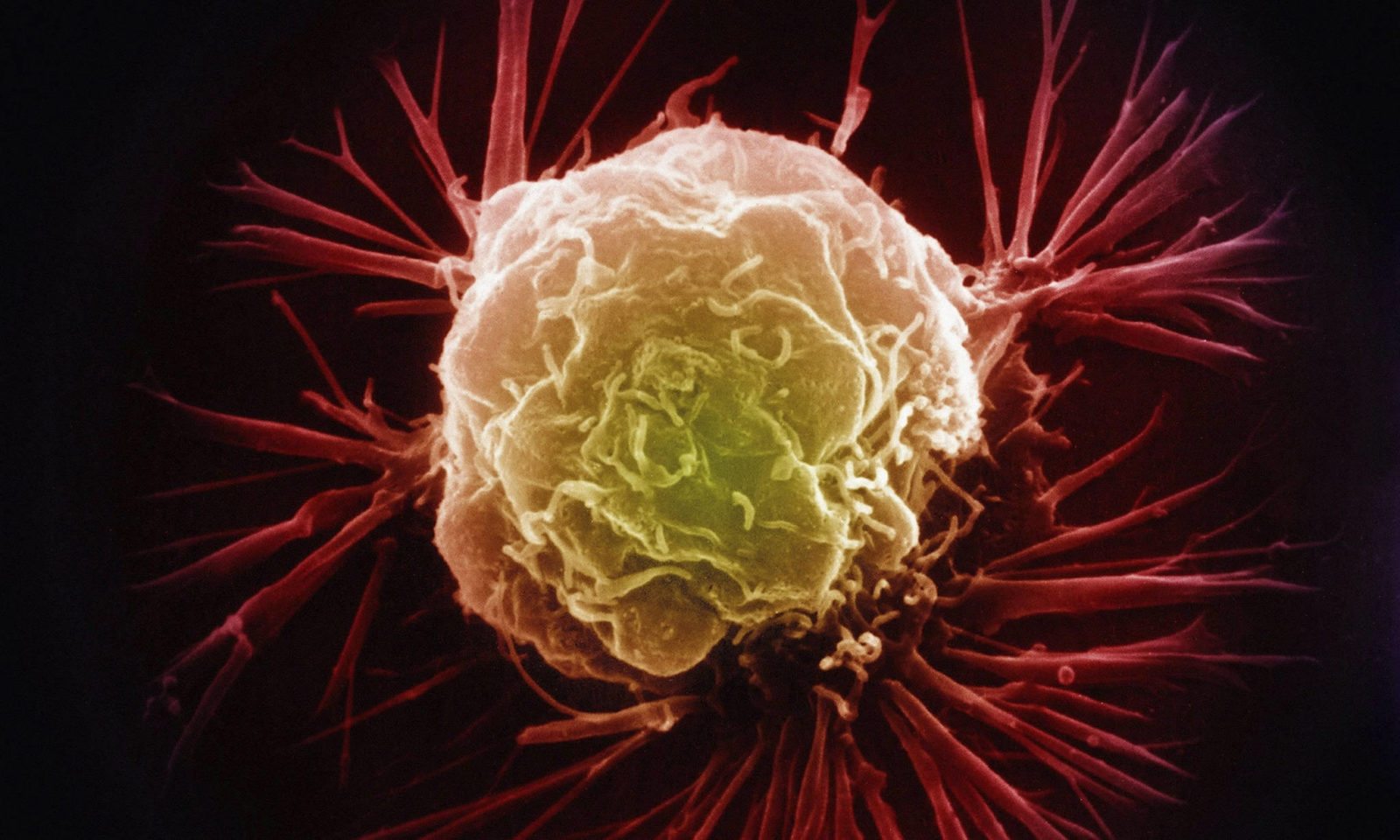
Complementary and Alternative Medicines and Cancer
Does complementary and alternative medicine offer any meaningful benefits to cancer patients?

CAM Promotion in Adolescent and Young Adult Cancer Programs
Cancer in the 18-39 age range is uncommon, but still occurs. When they should be dealing with school, friends, new jobs, and starting families, instead they must worry about medical bills, appointments, and infertility. Added to this are the costs of "integrative" treatments often foisted upon cancer patients, or built-in to the few adolescent and young adult-focussed centers that currently exist.

Rigvir: Another unproven and dubious cancer therapy to be avoided
Recently, the Hope4Cancer Institute, a quack clinic in Mexico, has added a treatment known as Rigvir to its coffee enemas and other offerings. But what is Rigvir? It turns out that it's an import from Latvia with a mysterious history. Proponents claim that it is an oncolytic virus that targets cancer specifically and leaves normal cells alone. Unfortunately, there is a profound...


