Tag: clinical trials

The FDA’s accelerated drug approval program is failing to protect cancer patients
Drug approval is a process that should be and, for the most part, is rooted in rigorous science. However, there is always a countervailing pressure to approve new drugs rapidly, particularly in cancer. That's why the FDA created the accelerated approval program in the early 1990s. Unfortunately, increasingly this approval process appears to be failing us in oncology. Reform is needed.
Naturopaths try (and fail yet again) to argue that they are science-based
That booster of all things "integrative," John Weeks has devoted the entire most recent issue of The Journal of Alternative and Complementary Medicine, which he edits, to trying to demonstrate that naturopathy is science-based. It does not go well. Same as it ever was.
Are antivaxers “holding science hostage”?
Melinda Wenner Moyer published an article in The New York Times arguing that fear of how antivaxers will react to scientific findings is leading scientists to self-censor. I'm not convinced that this is the case.

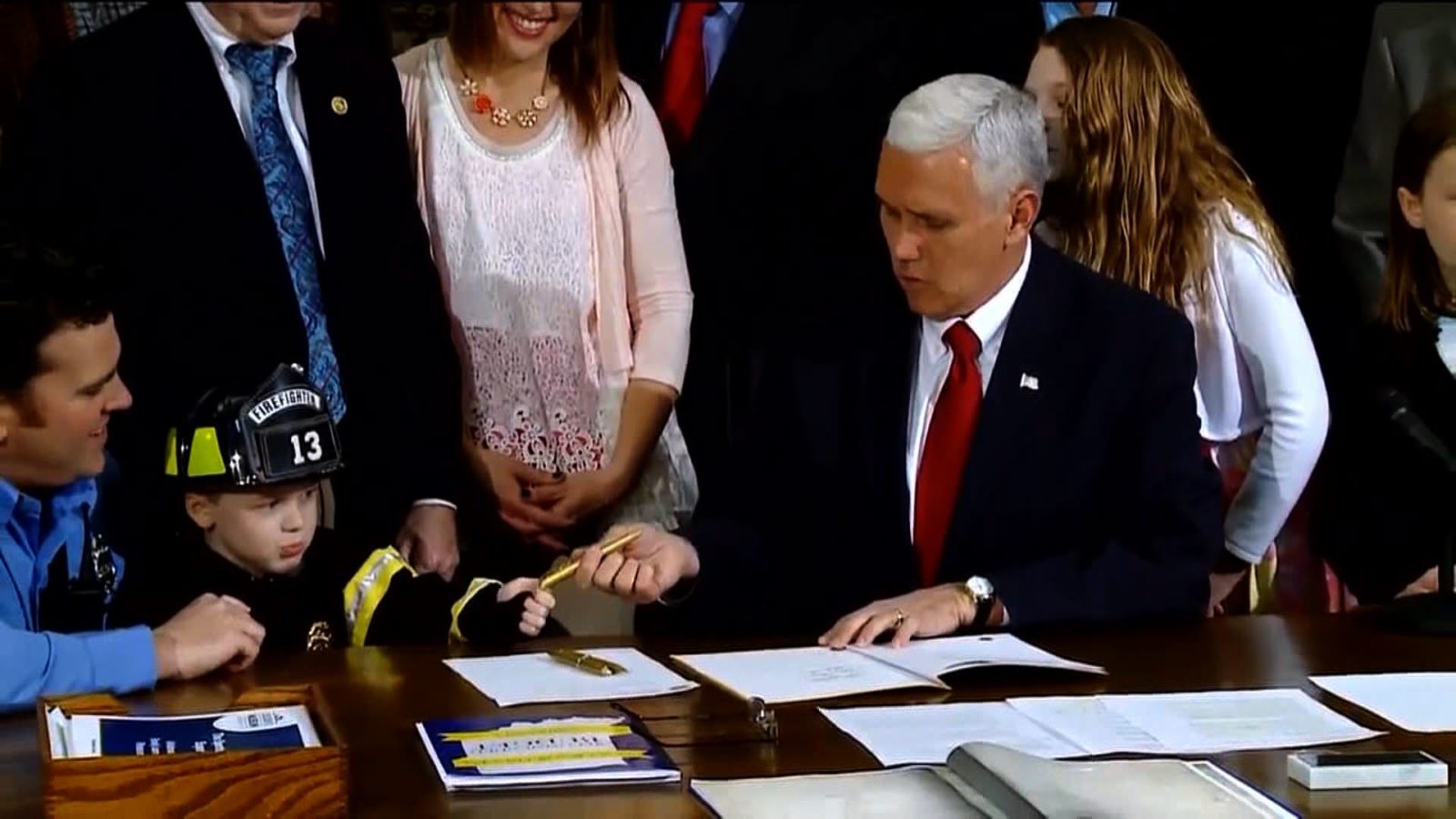
The very worst version of the sham known as “right-to-try” is poised to become law
"Right-to-try" laws are a cruel sham that purport to allow terminally ill patients access to promising experimental drugs. In reality, they strip away many protections and leave vulnerable patients on their own. After four years and a number of toothless state laws, a federal version of "right-to-try" is poised to become law. A version passed by the Senate could be voted on...

Essential Oils in the Ambulance
Aromatherapy with essential oils is pseudoscience, backed only with low quality studies guaranteed to show a placebo effect. Their growing popularity warns that better science education is needed.

Sen. Ron Johnson: Holding the bill funding the FDA hostage unless the cruel sham that is right-to-try is added to it
Advocates claim that "right-to-try" laws help terminally patients by allowing them access to experimental drugs before approval, when, in fact, such laws strip legal and regulatory protections from patients using such drugs and their purpose is actually to undermine and weaken the FDA. Now advocates led by Sen. Ron Johnson (R-WI) are making a new push to pass right-to-try by embedding it...

Bills remove impediments to ill-advised state “right to try” laws, shield wrongdoers, and hide adverse events
Congressional bills will unleash state "right to try" laws, block terminally ill patients from redress for damages caused by negligent doctors and drug companies, and hide adverse drug events from the public.
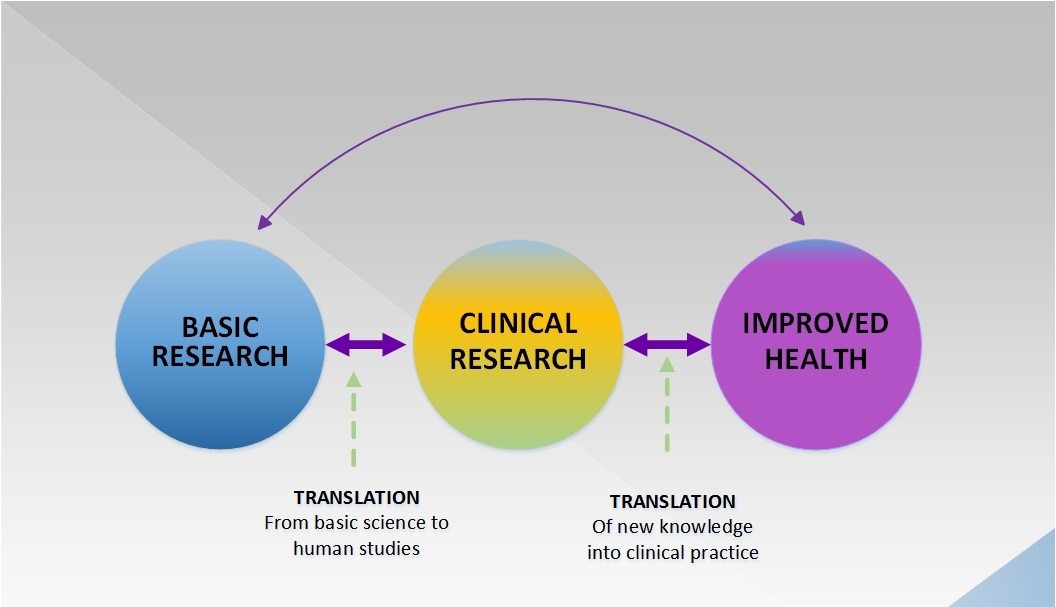
Donald Trump versus the FDA: Is the standard of evidence for drug approval actually too low rather than too high?
All of the candidates being considered by President Trump for FDA Commissioner believe that the FDA is too strict in its standards for approving new drugs. In a commentary in Nature last week, two bioethicists argued that, at least in terms of preclinical data, the standard of evidence is actually too low. Which is correct?


Responding to SBM Critics
A response to a critic of SBM, and setting the record straight on our actual positions regarding evidence and the practice of medicine.