Tag: ethics

To unblind or not to unblind? That is the question about clinical trials of COVID-19 vaccines
Antivaccine alternative health tycoon Joe Mercola claims that the unblinding of participants in the clinical trials of Moderna and Pfizer COVID-19 vaccines was intended to "blow up the trials" and undermine the science, making it impossible ever to identify long term adverse events. What he's really doing is deceptively oversimplifying complex ethical and scientific issues surrounding these trials in the middle of...
Is the use of “Open-Label” Placebo Ethical in the Treatment of Children?
Is the use of "open-label" placebo ethical in pediatric medical care, or any care for that matter? A recent article in Pediatrics discussing this issue comes to a flawed conclusion based on a misunderstanding of placebo and of the literature on placebo without deception.
Building a Case for CAM
[Editor’s note: Mark Crislip is taking a well deserved vacation from blogging, and James Thomas has kindly agreed to provide another guest post to fill the gaping need left in all of your lives. Enjoy!] According to the Orwellian-named National Center for Complementary and Integrative Health, roughly 33% of adults aged 18-44 and about 37% aged 45-64 use some form of CAM....
Is it ethical to sell complementary and alternative medicine?
Complementary and alternative medicine may be legal to sell - but is it ethical to sell?
The fine line between quality improvement and medical research
As I’ve mentioned before, the single biggest difference between science-based medicine (SBM) and what I like to call pseudoscience-based medicine, namely the vast majority of what passes for “complementary and alternative medicine” (CAM) or “integrative medicine” is that SBM makes an active effort to improve. It seeks to improve efficacy of care by doing basic and clinical research. Then it seeks to...

Antivaccine activists fund a study to show vaccines cause autism. It backfires spectacularly.
Having written about pseudoscience and quackery continuously for over a decade and having engaged in conversations about it online for over 15 years, I’ve come to recognize a number of traits that are virtually the sine qua non of quacks and pseudoscientists and their believers. Obviously, one of them is a severe case of the Dunning-Kruger effect, a tendency of those with...
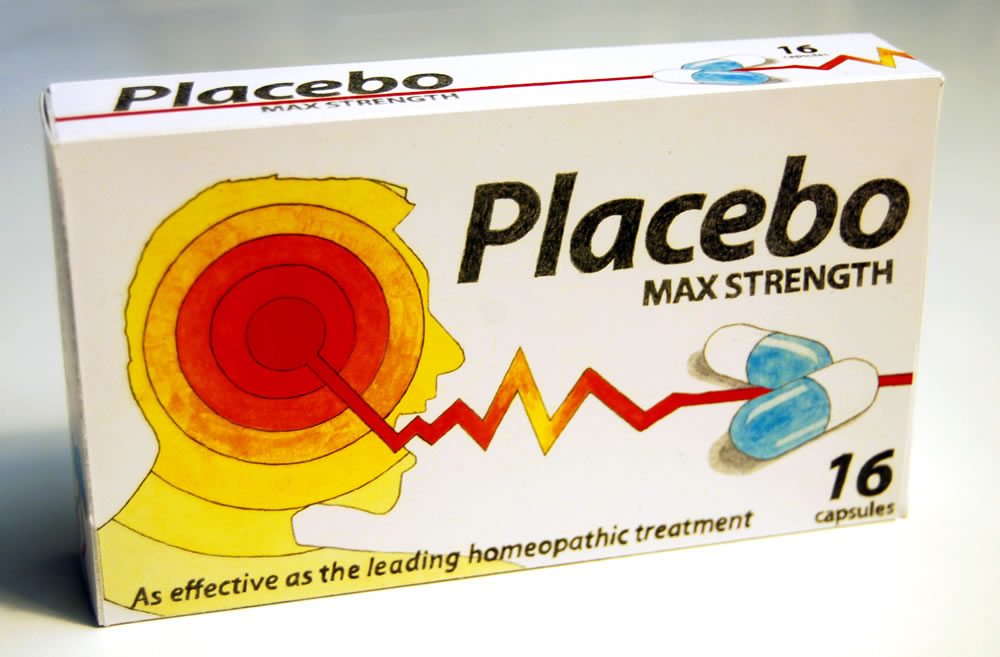
It’s time for pharmacies to stop selling sugar pills
Why are pharmacies selling sugar pills to consumers that are packaged like medicine? And what will it take for pharmacies to stop?
Selling complementary and alternative medicine: An business ethics perspective
Is it ethical to sell complementary and alternative medicine? This presentation — by a philosopher and a pharmacist — considers CAM from the perspective of commercial ethics.
Beware the Integrative Pharmacy
Imagine a retail pharmacy where some of the medicines on the shelves have been replaced with similar-looking packages that contain no active ingredients at all. There is no easy way to distinguish between the real and the fake. Another section of the store offers a number of remedies with fantastic claims, such as “boosting” the immune system, “detoxifying” the body, or “cleansing”...


