Tag: melanoma

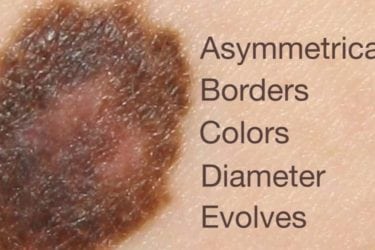
Melanoma: A Pseudoepidemic of Skin Cancer Prompts New Screening Recommendations
There appeared to be an epidemic of melanoma skin cancer, but it seems to be a pseudoepidemic caused by overdiagnosis. Screening everyone with skin exams does more harm than good and can no longer be recommended.
Do Sunscreens Cause Cancer?
Elizabeth Plourde thinks sunscreens cause cancer rather than preventing it. She blames sunscreens for everything from coral reef die-offs to autism. Neither her evidence nor her reasoning stand up to scrutiny.
Ty Bollinger’s “The Truth About Cancer” and the unethical marketing of the unproven cancer virotherapy Rigvir
Last week, I wrote about Rigvir, a "virotherapy" promoted by the International Virotherapy Center (IVC) in Latvia, which did not like what I had to say. When a representative called me to task for referring to the marketing of Rigvir using patient testimonials as irresponsbile, it prompted me to look at how Ty Bollinger's The Truth About Cancer series promoted Rigvir through...

Rigvir: Another unproven and dubious cancer therapy to be avoided
Recently, the Hope4Cancer Institute, a quack clinic in Mexico, has added a treatment known as Rigvir to its coffee enemas and other offerings. But what is Rigvir? It turns out that it's an import from Latvia with a mysterious history. Proponents claim that it is an oncolytic virus that targets cancer specifically and leaves normal cells alone. Unfortunately, there is a profound...
Clinical equipoise versus scientific rigor in cancer clinical trials
A critical aspect of both evidence-based medicine (EBM) and science-based medicine (SBM) is the randomized clinical trial. Ideally, particularly for conditions with a large subjective component in symptomatology, the trial should be randomized, double-blind, and placebo-controlled. As Kimball Atwood pointed out just last week, in EBM, scientific prior probability tends to be discounted while in SBM it is not, particularly for therapies...
How not to win friends and influence people
BLOGGER’S NOTE: The incident described in this post is true, although somewhat embellished to protect the names and identities of the innocent, if you know what I mean. This conversation occurred a few years ago at a large national cancer meeting. The question caught me by surprise. While attending a large national cancer meeting, I was having brunch with a friend, a...

