Tag: overtreatment

The Frenetic Frenum Freeing Frenzy
What problems do tongue-ties cause? Do all of them need to be clipped?

Osteopenia: When Does Decreased Bone Density Become a Disease Requiring Treatment?
Osteoporosis is routinely treated with bisphosphonates to prevent fractures. A new study suggests that osteopenia should be treated too. But questions remain.

PSA Screening for Prostate Cancer
PSA testing is controversial. A new study finds that PSA screening for prostate cancer offers no survival benefits.
How accurately do physicians estimate risk and benefit?
A new study suggests that physicians tend to overestimate the benefits of treatments, tests, and screening tests, while also underestimating harms.
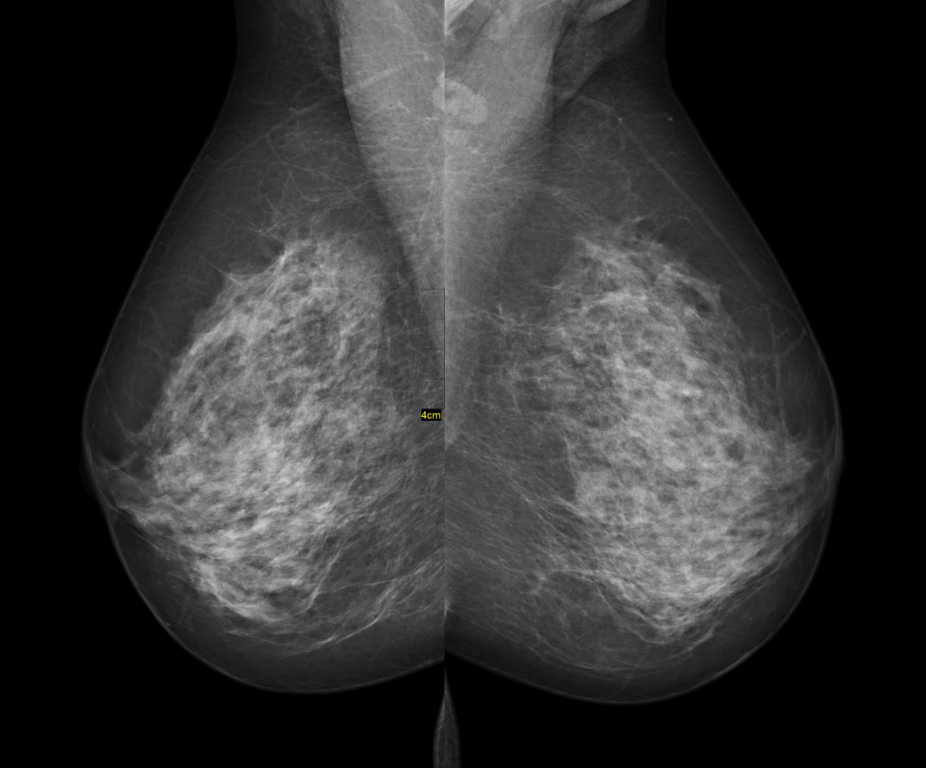
Mammography and overdiagnosis, revisited
Another new study supports the hypothesis that overdiagnosis is a major problem in mammography screening programs. Predictably, it is attacked based on a misunderstanding of what overdiagnosis is.

When science- and evidence-based guidelines conflict with patient wishes: What’s a doc to do?
We use the term "science-based medicine" (SBM) because medicine isn't a science. The best medicine, however, is based in science. Patient values are also important, but what is a science-based doctor to do when SBM conflicts with what a patient or family wants?
Confusing overdiagnosis for an “epidemic” of thyroid cancer in Japan after Fukushima
One of my favorite topics to blog about for SBM is the topic of overdiagnosis and overtreatment. These are two interrelated phenomena that most people are blissfully unaware of. Unfortunately, I’d also say that the majority of physicians are only marginally more aware than the public about these confounders of screening programs, if even that. Overdiagnosis has long been appreciated to be...

On “integrative medicine” and walking and chewing gum at the same time
Evidence matters. Science matters. However, when advocates of "integrating" quackery into medicine via the vehicle of "integrative medicine" invoke weak science and poor quality evidence in conventional medicine in response to criticism, what they are really doing is deflecting attention away from their quackery. More importantly, advocates of science-based medicine are capable of walking and chewing gum at the same time. We...

The American Cancer Society’s new mammography guidelines: Déjà vu all over again
One of the things that feels the weirdest about having done the same job, having been in the same specialty, for a longer and longer time is that you frequently feel, as the late, great Yogi Berra would have put it, déjà vu all over again. This is particularly true in science and medicine, where the same issues come up again and...
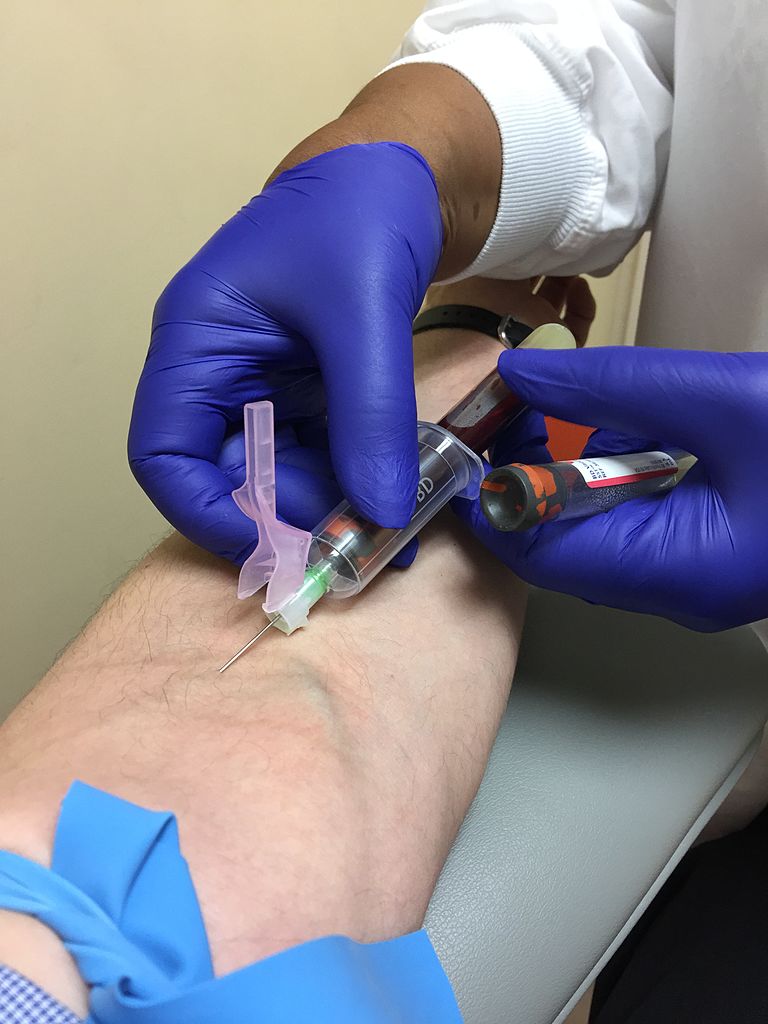
“Liquid biopsies” for cancer screening: Life-saving tests, or overdiagnosis and overtreatment taken to a new level?
I’ve written many times about how the relationship between the early detection of cancer and decreased mortality from cancer is not nearly as straightforward as the average person—even the average doctor—thinks, the first time being in the very first year of this blog’s existence. Since then, the complexities and overpromising of various screening modalities designed to detect disease at an early, asymptomatic...

