Tag: pain

Swearing to Treat Pain: Helpful Approach or Just Another Distraction
Pain is a complicated problem and something that we will all experience in our lives. Is swearing a helpful way to reduce pain, or is it just another distraction? Maybe it's both.
Poor Science Reporting and Premature Enthusiasm
Press releases often outpace the data. Here are some examples of over-enthusiastic reporting on extremely preliminary research.

Virtual Reality Therapy
Are virtual reality headsets a valid tool for treating back pain? Maybe.
Illness, Healing, and Other Terms That Can Be Confusing
Watch your language. Some terms that are frequently confused: pain vs. suffering, disease vs. illness, cure vs. healing. Science-based medicine focuses on diseases; alternative medicine focuses on illness: that explains a lot.

DNA Vibe Jazz Band
The DNA Vibe Jazz Band device promises to relieve pain and do other wonderful things. It has nothing to do with DNA, Jazz, or evidence.
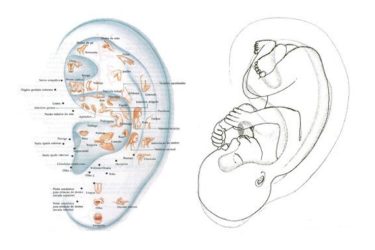
Ear Acupuncture for Procedural Pain in Neonates: More Randomized Controlled Nonsense
A recently published multicenter randomized and placebo controlled study attempted to answer the question of whether or not magnetic acupuncture beads stuck on premature baby ears reduced pain during a common screening exam. They don't. And they might have made things worse for these babies.

Rightful for Pain: Deceptive Advertising and a Dangerous Ingredient
Rightful is an herbal supplement mixture offering pain relief and much more. Its claims are deceptive and not backed by good science. Not only that, but one of its ingredients is contraindicated.

Salonpas
Salonpas is an over-the-counter topical NSAID used to treat pain. It's probably safe and might be worth trying for minor pain, but the effect is small and the advertising is more hype than substance.
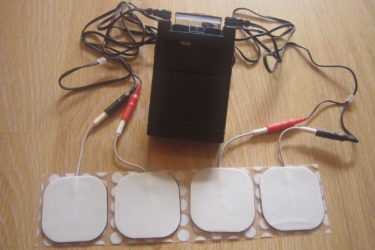
TENS for Pain Relief: Does It Work?
TENS units are used to relieve pain and for other indications. The evidence is not impressive.


