Chiropractors often deny that neck manipulation can be a primary cause of stroke by injuring vertebral arteries. But according to Jean-Yves Maigne, M.D., head of the Department of Physical Medicine at the Hôtel-Dieu Hospital in Paris, France:
It is now a well established fact that cervical thrust manipulation can harm the vertebral artery. This accident was formerly regarded as very rare, although severe, and related to atherosclerosis. Clinical tests were proposed to detect patients at risk. The problem is now better known. It is no longer attributed to atherosclerosis…but to a dissection of a vertebral artery, a clinical entity observed in younger patients (20-45 years). It remains very rare, but mild symptoms appear to be not so infrequent. Finally, the predicting tests seem to be deprived of any value.1
In 1997, the French Society of Orthopaedic and Osteopathic Manual Medicine (SOFMMOO), following presentations by anatomists, neurologists, radiologists, and practitioners in the field of French Manual Medicine, adopted the neck-manipulation proposals made by Dr. Maigne.1 “Acknowledging the fact that prevention is out of reach,” said Dr. Maigne, “the aim of these recommendations is to reduce the number of (not to say to suppress) rotational cervical thrust manipulations in a targeted population. This population consists mainly in females of less than 50 years old. Five recommendations were developed, in addition to classic contraindications of spinal manipulative therapy.”
The recommendations of the SOFMMOO, dealing with cervical manipulation in general and allowing the use of neck manipulation in special cases, are worth considering since they were reviewed by medical specialists in different disciplines and approved by licensed practitioners who use manual therapy, long before the stroke-neck-manipulation furor reached its peak in the United States.
Recommendations of the SOFMMOO
Recommendation #1: Seeking any undesirable effect following previous manipulative neck treatment such as nausea, headache, dizziness or vertigo. They could testify of a previous dissection with a favorable spontaneous outcome. This is an absolute contraindication to further cervical thrust manipulation.
Recommendation #2: No thrust manipulation for recent (i.e. acute) neck pain (less than 3-4 days), because it may be a symptom of a spontaneous dissection of the vertebral artery.
Recommendation #3: Neurologic exam mandatory before any cervical thrust (same reason as #2: the risk of a current dissection).
Recommendation #4: No cervical thrust in rotation in females less than 50 years. No cervical thrust in rotation in males less than 50 years at the first visit (but allowed at the second visit if the first treatment was not efficient). Instead of rotational thrust, it is highly recommended to use mobilizations, MET (muscle energy techniques), soft tissue cervical techniques and upper thoracic spine thrust manipulations (which certainly act on the cervico thoracic muscles).
Recommendation #5: Only physicians with a University Diploma passed at least one year before should be allowed to perform cervical manipulations. This latter recommendation should be adapted to the context of foreign countries. The idea is that a physician should not be allowed to thrust a neck without at least one year of full practice. Such an interval of time may allow him or her to feel comfortable and confident with other techniques (thoracic and lumbar spine).1
Why is upper cervical manipulation dangerous?
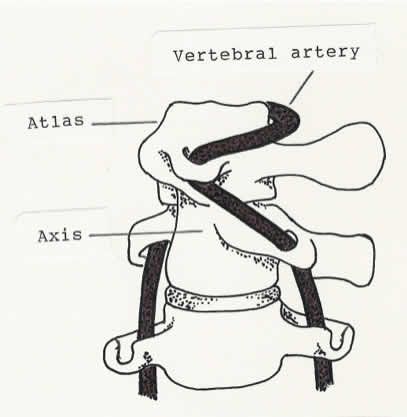
Extreme rotation of the atlas on the axis (at the atlantoaxial joint) stretches the vertebral artery.
Extreme rotation of the atlas on the axis (at the atlantoaxial joint) stretches the vertebral artery.
Although the incidence of stroke (and other complications such as injury to the carotid artery) caused by neck manipulation may be low, as indicated by the number of such strokes reported in insurance and hospital records, it seems likely that many strokes associated with neck manipulation are not recognized and reported as such. The symptoms of minor cases of dissection may be so slight and temporary that recovery takes place without recognition or treatment; some may be asymptomatic because of adequate collateral circulation. Regardless, the risk of stroke associated with neck manipulation cannot be denied. Case reports of post-manipulation strokes clearly suggest cause and effect, making it necessary to question use of neck manipulation except in very special cases that have multi-disciplinary approval.
It is generally accepted that neck manipulation is most dangerous when there is thrust-type manipulation with rotation in the upper cervical area.
The atlantoaxial joints (connecting the 1st and 2nd cervical vertebrae─the atlas and the axis) in the upper cervical area of the spine, where the greatest amount of rotation takes place, are most vulnerable to injury since there are no intervertebral disc fibers and no interlocking joints to limit rotation. The atlanto-occipital joints (forming the articulation between the atlas and the skull), designed primarily for flexion-extension (nodding of the head), fit together like cups sitting in saucers and are also without disc fibers and interlocking joints. Normally, during active cervical rotation, all of the cervical vertebrae move together, a little movement in each joint, allowing about 80 degrees of rotation right and left. The atlantoaxial joint, capable of about 50 degrees of rotation, is the only joint in the cervical spine where movement can occur alone, allowing excessive rotation when there is passive upper cervical rotation forced by a manual head contact or by specific contact on the atlas vertebra.
Because of the tortuous route of the vertebral arteries in the upper cervical area where they thread through the transverse processes of the atlas (1st cervical vertebra) and then make a sharp turn to travel behind the atlas and enter the skull through the foramen magnum (the opening at the bottom of the skull), extreme rotation of the skull or the atlas may place stress on the vertebral artery and the vertebrobasilar arteries that supply the brain with blood. Passive upper neck rotation forced by manual manipulation should not exceed 45 or 50 degrees if stroke-causing kinking or traumatic dissection of vertebral arteries is to be avoided. A head contact should not be used to force rotation of the neck. Sudden stretching of an atherosclerotic or fragile vertebral artery during a rapid manual rotation of the head might cause vertebral artery damage by overcoming the artery’s compromised elasticity, causing tears and bleeding in the intimal lining of the artery, releasing clots that may travel to the brain.
There is, of course, a vertebral artery on each side of the neck, threading up through the transverse processes of cervical vertebrae from C6 to C1. Extreme rotation of the atlantoaxial joint in either direction stretches both arteries to some degree, more on one side or the other, depending upon the direction of rotation.
Injury to weak or diseased vertebral arteries can occur as a result of such common activities as a beauty parlor shampoo or looking around to back a car out of a garage. But dissection of a healthy vertebral artery in a young person occurs as a result of trauma, such as that which might be caused by the high-velocity thrust of cervical manipulation that forces sudden, extreme rotation of the upper cervical vertebrae, primarily at the atlantoaxial joint. Needless to say, even though it is difficult or impossible to determine beforehand who has weak or defective vertebral arteries, spontaneous dissection does not excuse dissection caused or aggravated by unnecessary or inappropriate neck manipulation. Unfortunately, many chiropractors routinely manipulate (adjust) the neck to correct “subluxations.” Some are “upper cervical specialists” who believe that realigning the atlas will remove pressure on the brain stem and realign vertebrae from the neck down, often requiring a specific manipulative contact (a “chiropractic adjustment”) that forces isolated and abnormal movement of the atlas.
Mobilization of the cervical spine within a normal range of movement may be less damaging to vertebral arteries than the high-velocity low-amplitude thrust that moves joints past their normal range of movement. Of course, persons predisposed to stroke because of fragile or diseased vertebral arteries may sustain injury to a vertebral artery during cervical spine mobilization as well as during manipulation; patients should always be informed of such risk. The added risk of unnecessary thrust manipulation borders on malpractice. A 2010 Cochrane Database Systematic Review (January 20:1) reported that cervical manipulation was no more effective than mobilization in relieving neck pain. Obviously, whenever appropriate, the safer of two treatment methods should receive priority.
In special cases, manipulation that produces cavitation (movement of joints into the paraphysiologic space where slight separation of joint surfaces occurs, often producing a popping sound) might be more effective than mobilization in restoring mobility and improving range of motion in previously injured joints. With proper manipulative contact, mid and lower cervical vertebrae can be rotated to produce cavitation or separation of joint surfaces without rotating the atlantoaxial joints. It’s possible to produce cavitation in the upper cervical joints without exceeding 50 degrees of rotation if certain manipulative-traction techniques are used. But except in very rare cases, I suspect that risk would outweigh benefit.
Contraindications for manipulating the neck
It seems unlikely that upper cervical manipulation could be totally banned, as some stroke-prevention advocates have proposed, since there may be rare problems involving the atlanto-occipital and atlantoaxial joints that could benefit from special manipulative techniques that do not involve excessive rotation. In the absence of a complete ban on the use of upper cervical manipulation, there are some contraindications to be considered. It goes without saying that sudden appearance of neck pain for no known reason, persistent undiagnosed neck pain, or neck pain immediately following injury should not be treated with manipulation, nor should disc herniation or nerve root impingement. Signs of vascular insufficiency, such as dizziness or fainting that occur during active or passive rotation or extension of the neck, or carotid artery bruits (noise caused by turbulent blood flow, often associated with atherosclerosis) heard on auscultation, would certainly be a red flag. Undetected vertebral artery fragility entails some degree of risk in any kind of neck manipulation, requiring that such treatment be used only as a last resort and only with informed consent.
Once the cause of neck pain has been diagnosed (ruling out structural abnormality, pathology, and vascular insufficiency), some types of uncomplicated mechanical-type neck pain might benefit from manipulation. Some diagnoses will strictly prohibit manipulation of the cervical spine. Rheumatoid spondylitis, for example, primarily affects the cervical spine and can cause atlantoaxial instability or true atlas subluxation that should not be manipulated. In rare cases, congenital absence of the odontoid process (a dowel-like projection of the axis that guides rotation of the atlas) will greatly weaken the atlantoaxial joint, making it more vulnerable to injury. Abnormalities in the upper cervical area may be associated with hidden nerve and vascular problems, such as an Arnold-Chiari malformation in which there is hypermobility (ligament weakness) in the atlanto-occipital and atlantoaxial joints with extension of cerebellar brain into the spinal canal. Arnold-Chiari may be associated with syringomyelia, a fluid-filled, vascular-rich cyst in the spinal cord that can be disturbed by manipulation. Basilar invagination, caused by softening of bone at the base of the skull, allows upward movement of the axis odontoid process into the foramen magnum, narrowing this opening at the base of the skull and encroaching upon the brain stem. Obviously, manipulation of upper cervical structures is a potentially dangerous procedure, requiring serious consideration and careful screening to rule out disease, genetic bone disorders, and other relevant problems.
Most neck problems can be treated better by time, massage, traction, exercise, and physical therapy modalities than by thrust manipulation. When neck manipulation is considered for treatment of an ongoing neck problem that has not responded to mobilization and conventional treatment methods, an x-ray exam should be done to rule out pathology and bony malformations before the manipulation is done. An MRI might be needed to find such conditions as an Arnold-Chiari malformation, depending upon the patient’s symptoms.
“Subluxation”: The most common reason for unnecessary neck manipulation
A diagnosis of “chiropractic subluxation,” alleged to be a cause of a great variety of ailments (requiring that every patient have neck manipulation), is a red flag and a major contraindication for neck manipulation since it can lead to excessive, inappropriate, and unnecessary manipulation, posing a risk of stroke. A subluxation diagnosis attached to an organic problem automatically precludes a correct diagnosis. Although a real orthopedic subluxation (not the same as an imaginary, asymptomatic chiropractic subluxation) can cause mechanical-type neck pain, it is not uncommon for chiropractors to report that subluxations are involved in every type of neck pain. A common neck crick (muscle spasm), for example, the kind a healthy person wakes up with in the morning, is usually a self-limiting condition that will resolve in several days with or without treatment if there is not a history to indicate a pre-existing problem caused by disease or injury. Chiropractors who inform their patients that subluxations cause neck cricks commonly take credit for curing this problem, leading the patient to believe that ongoing treatment is needed to keep subluxations from recurring and to prevent the development of illness, even when there are no symptoms. I always advised my patients to leave their neck alone if it is not bothering them and to avoid treatment by chiropractors who routinely manipulate (adjust) the neck to correct “subluxations.”
Although informed consent should be obtained from every patient who submits to neck manipulation, informed consent does not justify unnecessary neck manipulation and its concomitant risks.
References
Vautravers P, Maigne JY. Cervical spine manipulation and the precautionary principle. Joint Bone Spine. 2000;67:272-6. Accessed July 6, 2014 .

Sam Homola is a retired chiropractor who has been expressing his views about the benefits of appropriate use of spinal manipulation (as opposed to use of such treatment based on chiropractic subluxation theory) since publication of his book Bonesetting, Chiropractic, and Cultism in 1963. He retired from private practice in 1998. His many posts for ScienceBasedMedicine.org are archived here.
