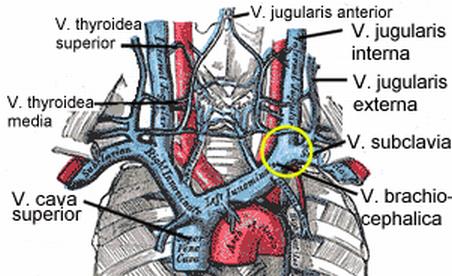
Diagram of the veins of the neck, including the jugular, which are claimed to cause multiple sclerosis through chronic cerebrospinal vascular insufficiency.
There is an interesting controversy raging in the multiple sclerosis (MS) world that reflects many of the issues we discuss at science-based medicine. Dr. Paolo Zamboni, and Italian vascular surgeon, has now published a series of studies claiming that patients with clinically defined MS have various patterns of chronic cerebrospinal venous insufficiency (CCSVI). Further Dr. Zamboni believes CCSVI is a major cause of MS, not just a clinical side-consequence, and is exploring treatment with venous angioplasty or stenting.
The claims have captured the attention of MS patients, many of whom have a progressive course that is only partially treated by currently available medications. There are centers popping up, many abroad (such as India), providing the “liberation procedure” and anecdotes of miraculous cures are spreading over the internet. There is even a Facebook page dedicated to CCSVI, and you can read the anecdotes for yourself. Many profess dramatic improvement immediately following the procedure, which seems unlikely even if Zamboni’s hypothesis is correct.
Zamboni is also getting attention from neurologists and MS specialists, who remain skeptical because Zamboni’s claims run contrary to years of research and thousands of studies pointing to the current model of MS as an autoimmune disease.
Dueling narratives
There are at least two stories to follow here. The first is the scientific story – the questions being proposed are answerable with scientific research, and they will be answered. MS remains a serious illness that is inadequately treated (not to downplay the important advances we have made, but we certainly are far from an adequate cure for MS). The potential of a new treatment deserves serious research attention, and CCSVI is getting it. It will probably take another ten years for the research to play itself out adequately for there to be a confident consensus on CCSVI, but eventually we will have a scientific answer.
The other story is the reaction of the public and the MS community. This has been mixed, but already there are conspiracy theories that the neurology community, the MS society, and Big Pharma (of course) are fighting against CCSVI as part of a misguided turf war. (See the comments to my previous posts on this topic at NeuroLogica for some examples.) Anecdotes are being used to argue against published scientific evidence, and negative studies are being dismissed. If CCSVI is eventually found to be a scientific dead end, I have to wonder if it will survive as just another fringe “alternative” treatment, like Laetrile, psychomotor patterning, and other discarded ideas in medicine.
The scientific story
So far there is not much of a scientific story to tell. A PubMed search on CCSVI yields a total of 19 publications (a pittance), indicating how new this concept is. I suspect this number will grow into the hundreds at least before this story plays itself out. If CCSVI is proven to be legitimate then this number will grow into the thousands over the next few decades. If it is disproved, publications will trickle off.
Most of the current research is published by Zamboni’s team. He is building an impressive list of studies, exploring various aspects of CCSVI and MS, but evidence that derives entirely from a single research team is always suspect. The role of bias in research is well documented, and further most new ideas in medicine turn out ultimately to be wrong. Therefore skepticism is the proper approach to bold new claims being supported by a lone research team. Replication will be necessary for the broader scientific community to take CCSVI seriously.
The core claim made by Zamboni is that most patients with MS display two or more out of five criteria on studies of venous anatomy (using ultrasound or venography) of venous insufficiency, while control patients (healthy subjects or those with other neurological disorders) display one or no criteria, and never two or more. All other claims (benefit from angioplasty, matching patterns of venous insufficiency with types of MS) derive from this core claim.
I found four independent replications in the literature, three very recently published. The first is by Al-Omari MH, Rousan LA, who found:
According to the described criteria, 92% of the MS patients showed abnormal findings and 84% of them showed evidence of CCSVI, however; only 24% of controls showed abnormal findings, but none of them showed evidence of CCSVI (OR=7.25, 95% CI 2.92-18.01, P<0.0001).
These are similar numbers to Zamboni, although the 84% is a little less. This study used only ultrasound, which is a non-invasive technique and therefore good for screening, but the results are very operator-dependent. There is no indication in the study that the patients were assessed in a blinded fashion.
The next study by Florian Doepp et al used the following methods:
We performed an extended extra- and transcranial color-coded sonography study including analysis of extracranial venous blood volume flow (BVF), cross-sectional areas, IJV flow analysis during valsalva manoever (VM) as well as ‘CCSVI’ criteria. 56 MS patients and 20 controls were studied.
They found no subjects met the Zamboni criteria for CCSVI – a completely negative replication.
The second was performed by Krogias et al., who found:
The authors conclude that the “chronic cerebrospinal venous insufficiency (CCSVI)” cannot represent the exclusive pathogenetic factor in the pathogenesis of MS. In our cohort, only 20% of the patients fulfilled the required neurosonological features of CCSVI. So far, the pathogenetic relevance of these findings remains speculative. Thus, based on the current scientific position we cannot justify invasive “therapeutic” approaches, especially if they are performed outside of clinical trials.
The third study is a Swedish study by Sundström et al., “Venous and cerebrospinal fluid flow in multiple sclerosis – a case-control study.” This study used MRI scanning to assess blood flow in the internal jugular vein in 21 MS patients and 20 controls, and found no difference.
Conclusion: A small but telling body of results
One of four replications found results similar to Zamboni. A second found only 20% of MS patients met Zamboni’s criteria, while two others found that no patients with MS did. Four studies are not a lot – and are not even close to ending this controversy from a scientific point of view. But these early results are not promising and will tend to deepen skepticism within the neurological community.
Clearly there is a need for more research so that both patients and professionals can feel comfortable that CCSVI has been given a thorough investigation and we can say with confidence what role, if any, it plays in MS. The results, also, do not have to be black and white. While it seems unlikely that Zamboni has discovered the sole and ultimate cause of MS in most or all patients, it is possible he has found a significant consequence of MS. Chronic inflammation may result in venous insufficiency in some patients. This venous insufficiency may further play a role in worsening the clinical course in a subset of those patients, who may benefit from treatment. So CCSVI may ultimately play a minor but important role in the management of MS.
Or it may all turn out to be a figment of Zamboni’s imagination, spawned by the sincere hope of finding a cure for MS. Time and research will tell.
My open plea to the MS community, especially those who are going down the rabbit hole of conspiracy theories, is to keep this discussion about the scientific evidence. This is not the place for cheap conspiracy theories. I fear my plea will fall on deaf ears, but it never hurts to ask.
