One of the concepts we often discuss around here is “what is disease?” As we’ve seen in the discussion of Lyme disease and so-called Morgellon’s syndrome, this is not always an easy question to answer. Knowing what states are disease states does not always yield a black-or-white answer. The first step is usually to define what a disease is. The next problem is to decide who in fact has that disease. The first question is hard enough, especially in disease states that we don’t understand too well. The second question can be equally tricky. To explore the scientific and philosophical issues of diagnosing an illness we will use as a model diabetes mellitus (DM). This won’t be quite as boring as you think, so don’t click away yet. (Most of the information here refers more specifically to type II diabetes, but most of it is valid for type I as well.)More…
Diabetes
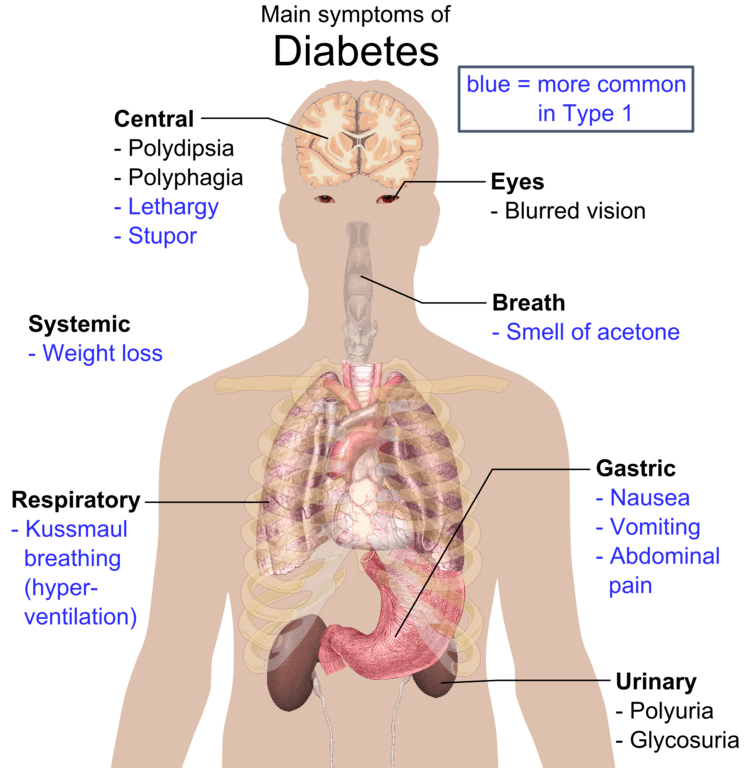
Diabetes is a metabolic disorder characterized by elevated blood sugar levels. Sometimes very high sugar levels can lead to illness and death, such as in diabetic ketoacidosis. These days, however, people rarely die from having a high blood sugar. The elevated blood sugars of diabetes cause a host of changes in the body over time, leading to two main types of problems: microvascular complications such as blindness and kidney failure, and macrovascular complications such as heart attack and stroke. The macrovascular problems are not unique to diabetics, but the microvascular complications, such as diabetic retinopathy (DR) are unique, and a good ophthalmologist can identify a likely diabetic without even checking a blood sugar level. But blood sugar levels are how we designate someone as being diabetic.
Who is diabetic?
Having diabetes puts you at high risk for the medical complications listed above. Intervening medically can reduce these risks, so knowing who is and is not diabetic is rather important. But knowing who is diabetic is not immediately obvious. Currently, the most accepted way of diagnosing someone as being diabetic is by checking a fasting blood sugar level. But blood sugar levels a very labile. It’s not clear how well blood sugar levels correlate to the risks of diabetes. This week, the journal Diabetes Care released new guidelines from the International Expert Committee which has been tasked with examining how we decide who is, in fact, diabetic.
The damage done by high blood sugars happens over time, but a blood sugar level is a brief snapshot. What clever researchers have done in the past is evaluate patients for a common complication, diabetic retinopathy, and correlate this with blood sugar values. These studies have helped us to decide who is diabetic, as they have shown us that above a certain level, a doctor can see the retinal changes of diabetes. But using a single blood sugar measurement can miss many people who are at risk for diabetes complications.
A test we’ve used for years to monitor the long-term control of blood sugar is the glycosylated hemoglobin level (HbA1C). Hemoglobin, the molecule in red blood cells that carries oxygen, will change when exposed to high blood sugar levels. Normally, about 5% of your hemoglobin is glycosylated, that is, attached to sugar molecules. These A1C molecules reside in red blood cells whose average life span is 120 days, so A1C levels generally reflect about three months of blood sugar levels.
Studies have shown that A1C levels over 6.5-7.0% are associated with increasing complications from diabetes. The International Committee reviewed the data on blood sugar as it relates to A1C, and both A1C and blood sugar as they relate to DR. They found that an A1C of 6.5% and above is closely associated with DR. Therefore, they recommend defining diabetes as having an A1C of 6.5% or above.
Implications
Changing the way we diagnose diabetes does a few things. First, it recognizes that clinicians have been using A1C levels to “diagnose” diabetes for years. It then examines this practice and finds that what we’ve been doing likely prevents diabetic complications. The other effect it will have is to “increase” the number of diabetics as we capture more diabetics with improved testing.
This is a wonderful example of how science-based medicine works. First, a plausible hypothesis is formed (A1C levels should correlate with physical changes in diabetics), looks at the evidence (A1C levels correlate well with diabetic retinopathy), and then practice recommendations are made.
Most important, however, is the realization that practice must change if the evidence warrants. This ability to change is the fundamental difference between medicine based on science, and everything else.
Reference
The International Expert Committee (2009). International Expert Committee Report on the Role of the A1C Assay in the Diagnosis of Diabetes Diabetes Care DOI: 10.2337/dc09-9033
