
Antivaccine propaganda from Dr. W. Gifford-Jones in The Toronto Sun
On Saturday, The Toronto Sun published a syndicated column by a pseudonymous Canadian doctor, Dr. W. Gifford-Jones. The column was packed with antivaccine misinformation and pseudoscience. Apparently due to complaints, the article was taken down sometime Sunday, but is still available on the websites of several other Canadian newspapers. Its misinformation is still there to frighten parents out of vaccinating.

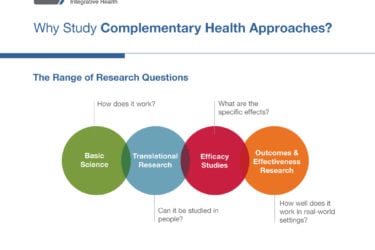
The Integrative Oncology Scholars Program: Indoctrinating the next generation of “integrative oncology” believers
"Integrative oncology" involves "integrating" pseudoscience, mysticism, and quackery with science-based oncology and co-opting science-based lifestyle modalities as "alternative" in order to provide cover for the quackery. Unfortunately, my alma mater, funded by the National Cancer Institute, is running a course to indoctrinate 100 health care professionals in the ways of "integrative oncology." The Trojan horse of "lifestyle interventions" and "nonpharmacologic treatments for...

My Cancer Free Life: A reality series designed to promote Stanislaw Burzynski’s quackery
Stanislaw Burzynski has been selling a dubious treatment known as antineoplastons to desperate cancer patients since the late 1970s. Unfortunately, there are those who are all too willing to promote the myth of a Brave Maverick Doctor who can cure cancer. Several years ago, it was Eric Merola. Now it's Uchenna Agu, a reality TV star turned producer. He plans on making...

Cancer disparities: It’s money that matters (along with a lot of other things)
Cancer is a complex set of diseases. I commonly discuss complexities in its biology and treatment. However, there's another layer of complexity that leads to marked disparities in cancer incidence and death rates. One major factor associated with such disparities is socioeconomic status.

A whole issue of JACM devoted to “integrative oncology” propaganda? Oh, goody.
Last week, The Journal of Alternative and Complementary Medicine published a Special Focus Issue on "integrative oncology." In reality, it's propaganda that promotes pseudoscience and the "integration" of quackery into oncology.

Crowdfunding: The fuel for cancer quackery
Ever since I first started taking notice about cancer quacks like Stanislaw Burzynski, I noticed how crowdfunding using social media and sites like GoFundMe appear to be an integral part of the business model of quack clinics. Thanks to an investigation by The Good Thinking Society published in BMJ last week, I now have a feel for the scope of the problem....
Acupuncture versus breast cancer treatment-induced joint pain: Spinning another essentially negative study
The investigators behind a recent clinical trial testing acupuncture to treat joint pain caused by aromatase inhibitors used to treat breast cancer are spinning it as a positive study. As is usually the case for acupuncture studies. It isn't
NCCIH has a new director, and she’s a true believer in acupuncture.
Helene Langevin has been named the new director of the National Center for Complemenary and Integrative Health. Given her history of dodgy acupuncture research, my prediction is that the quackery will flow again at NCCIH, the way it did in the 1990s when Tom Harkin zealously protected it from any attempt to impose scientific rigor.

Bait and switch in Oregon: Substituting quackery for opioids for Medicaid patients
The Oregon Health Authority is on the verge of passing a radical policy that would require chronic pain patients receiving Medicaid to have their opioids tapered to zero while covering "nonpharmacologic treatments for pain" that include primarily acupuncture, chiropractic, massage therapy, and other "alternative" treatments. Not surprisingly, the Oregon Chronic Pain Task Force, which is responsible for this proposed infliction of quackery...


