Why take a drug, herb or any other supplement? It’s usually because we believe the substance will do something desirable, and that we’re doing more good than harm. To be truly rational we’d carefully evaluate the expected risks and benefits, estimate the overall odds of a good outcome, and then make a decision that would weigh these factors against any costs (if relevant) to make a conclusion about value for money. But having the best available information at the time we make a decision can still mean decisions turn out to be bad ones: It can be that all relevant data isn’t made available, or it can be that new, unexpected information emerges later to change our evaluation. (Donald Rumsfeld might call them “known unknowns.”)
As unknowns become knowns, risk and benefit perspectives change. Clinical trials give a hint, but don’t tell the full safety and efficacy story. Over time, and with wider use, the true risk-benefit perspective becomes more clear, especially when large databases can be used to study effects in large populations. Epidemiology can be a powerful tool for finding unexpected consequences of treatments. But epidemiologic studies can also frustrate because they rarely determine causal relationships. That’s why I’ve been following the evolving evidence about calcium supplements with interest. Calcium supplements are taken by almost 1 in 5 women, second only to multivitamins as the most popular supplement. When you look at all supplements that contain calcium, a remarkable 43% of the (U.S.) population consumes a supplement with calcium as an ingredient. As a single-ingredient supplement, calcium is almost always taken for bone health, based on continued public health messages that our dietary intake is likely insufficient, putting women (rarely men) at risk of osteoporosis and subsequent fractures. This messaging is backed by a number of studies that have concluded that calcium supplements can reduce bone loss and the risk of fractures. Calcium has an impressive health halo, and supplement marketers and pharmaceutical companies have responded. There are pills, liquids, and even tasty chewy caramel squares embedded with calcium. It’s also fortified in foods like orange juice. Supplements are often taken as “insurance” against perceived or real dietary shortfalls, and it’s easy and convenient to take a calcium supplement daily, often driven by the perception that more is better. Few may think that there is any risk to calcium supplements. But there are now multiple safety signals that these products do have risks. And that’s cause for concern.
Calcium is a critically important mineral for body function. It’s not only the major building block in bones, it’s required for muscle contraction, blood clotting, and multiple hormone and neurotransmitter actions. Vitamin D function is closely linked with dietary calcium absorption and its activity in the body, and also facilitates the exchange of calcium to and from bone “stores”. The dietary importance of both vitamin D and calcium have been acknowledged and recommended daily intakes have been established for both agents.
Calcium and vitamin D have been studied extensively because the burden of illness from osteoporosis is so great. Almost 50% of all women over the age of 50 will have an osteoporosis-related fracture. And fracture can mean significant, sometimes permanent decreases in quality of life, increasing the odds of ending up in a long-term care facility, and raising mortality risks dramatically.
About two years ago I asked if calcium supplements were causing heart attacks. New studies were raising questions about efficacy and safety, which was worrying. Some older data had pointed to the potential relationship. In 2010 Bolland et al. published a meta-analysis of all randomized controlled trials of calcium supplements (≥500 mg/day), excluding trials that also gave vitamin D concurrently. Two sets of data were analyzed: those with patient-level data, and those with trial-level data. Both data sets, when analyzed, showed an association of calcium supplement consumption with increased rates of heart attacks — the relative risk increase was about 30%. There was some fair criticism of the analysis after it was published — the studies were never designed or intended to assess cardiovascular events as primary endpoints; a composite endpoint was not significant; and the exclusion of studies of calcium given with vitamin D made the value questionable, given treatment is now typically with both products. Bolland subsequently addressed the vitamin D question with the (161,000 patient) Women’s Health Initiative dataset, and added in two other trials that studied calcium and vitamin D. Once again, he observed a significant increase in heart attacks. Finally he combined all the data into one overall risk estimate: calcium alone, and calcium with vitamin D. The association was still present and statistically significant: A 24% relative risk increase for heart attacks in those that take calcium supplements.
In light of the warning signals, I suggested two years ago that caution be exercised with calcium supplements, and that routine supplementation in the absence of a dietary deficiency was inadvisable. Furthermore, given no harms had been shown with dietary intake, that all possible efforts should be made to maximize intake by that route. Finally, I suggested that in the case of dietary deficiency, that the potential risks of therapy be considered, along with the expected benefits. Given the modest benefit of calcium supplementation on real outcomes, like fracture risks, the cardiovascular warning signals were concerning enough that they should factor into treatment decision-making.
That was 2011. There’s new data and new guidance on calcium supplements. And the risk and benefit perspectives have shifted again.
In 2012 Li and colleagues examined a group of Heidelberg, Germany residents enrolled in the publicly-funded European Prospective Investigation into Cancer and Nutrition study. Like Bolland, the goal was to evaluate the relationship between dietary calcium, calcium supplements, and cardiovascular events like heart attacks and strokes. Participants were asked if they took vitamins and supplements regularly — dosages were not recorded. Over 23,000 patients were examined for an average duration of 11 years, and 354 heart attacks, 254 strokes, and 267 cardiovascular-related deaths were reported by participants and confirmed by examining medical records. A long list of potential confounders were adjusted for, including total dietary calcium intake, consumption of anti-inflammatory drugs, and reported high cholesterol levels, in order to isolate the potential association of supplements with any cardiovascular benefits.
There were significant differences between the groups, which complicates the interpretation. Consuming higher levels of dietary calcium was associated with a number of other factors including younger age, more education, more physical activity, less smoking and less alcohol consumption. Supplement users were more likely to be women, more active, and less likely to be overweight. However there was more smoking and less education in this group. Controlling for these factors, the authors observed the following:
- Dietary calcium intake did not appear to affect the risk of cardiovascular disease. When consumption was divided into four groups by total intake, the third quartile had fewer cardiovascular events than the lowest quartile. The risk for stroke was increased in the second quartile for two years, then disappeared. Overall, there was no clear pattern observed.
- Calcium supplement consumptionwas associated with more heart attacks, but not strokes or overall cardiovascular death. The observed rise in heart attack risk was substantial and statistically significant (hazard ratio of 1.86, confidence interval of 1.17-2.96). This elevated risk was even higher in calcium-only supplementers, where a 2.39x elevated risk was observed (confidence intervals 1.12-5.12).
There were a number of important limitations to the conclusions, a notable one being that calcium supplement doses were not collected. However, the large population, long duration of study, and confirmation of all outcomes, like heart attacks and deaths, supports the credibility of the analysis. The lack of association between dietary calcium (dairy and non-dairy) and cardiovascular death is reassuring. On the other hand, the relationship between calcium supplements and heart attack risk is consistent with the Bolland meta-analyses, and troubling. We now have different authors studying a different dataset and identifying the same signal,which strengthen the hypothesis that this association is real.
Next we have an analysis by Xiao and associates. The study, Dietary and Supplemental Calcium Intake and Cardiovascular Disease Mortality was published in JAMA Internal Medicine in February 2013. It also used a massive cohort of patients, pulling data on almost 400,000 adults enrolled in the NIH-AARP Diet and Health Study. This study started in the mid-1990’s and assessed dietary and supplemental calcium intake over 12 years of follow-up. Calcium supplements were taken by about a quarter of all men and over half of all women. Again, there were differences between calcium supplement users from non-users: They were more likely to be non-Hispanic whites, to have more education, to be active, to rate their health as “excellent”, and to eat more fruits, vegetables and whole grains. Supplement users were less likely to smoke and consumed less alcohol.
They found the following:
- Calcium intake as supplements (>1000mg/day) by men was associated with a 20% elevated risk of cardiovascular death, due to an increased incidence of heart disease (confidence intervals 1.05-1.36). There was no effect on rates of stroke.
- Supplemental calcium intake by women was not associated with cardiovascular death. There was a slight but non-significant increase in supplement users compared with nonusers.
- There was no relationship of dietary calcium intake to cardiovascular death in men or women.
Once again, the lack of any association between dietary calcium intake and cardiovascular disease adds strength to the findings in other studies. Some reassurance, but more questions. The association with cardiovascular death in men only, but not women, is puzzling. Is the association real? My personal sense is that the association identified by Bolland looks more real than it did two years ago, despite the Xiao findings. So while we don’t have consistent evidence of harm, we do see an association that probably should not be ignored.
So what’s the role of calcium supplements? If it comes down to an evaluation of risk and benefit, where does calcium supplementation fit?
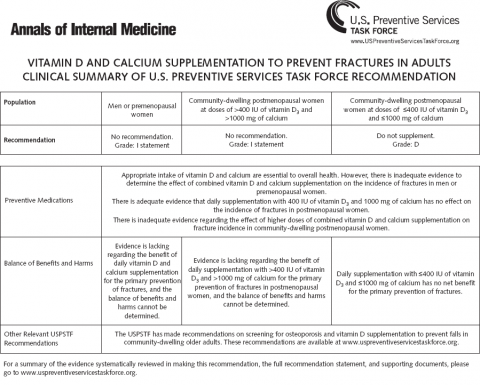
Two days ago the Vitamin D and Calcium Supplementation to Prevent Fractures in Adults: U.S. Preventive Services Task Force Recommendation Statement was published. As should be clear from the name, the USPSTF makes recommendations about prevention — not treatment. It does not consider cost, but only benefit and harms. This was an analysis that looked at primary prevention — the supplementation for adults (community dwelling, not hospitalized) for bone health in the absence of confirmed osteoporosis or a vitamin D deficiency. It did not look at the appropriate dietary intake levels, or the effects of calcium supplements alone. It also did not consider outcomes unrelated to bone health such as prevention of falls, cardiovascular disease, or overall mortality. Consequently, the data set studied by the USPSTF excluded the studies discussed above. With respect to cardiovascular outcomes, it remarks that the association of harms is “not consistently demonstrated”.
The new statement reflects the findings of two systematic reviews and a meta-analysis which sough to understand the relationship between vitamin D, calcium, bone outcomes like fractures, and adverse effects of taking supplements.
With respect to the net benefits of supplements, it made the following observation:
Except for postmenopausal women, there is inadequate evidence to estimate the benefits of vitamin D or calcium supplementation to prevent fractures in noninstitutionalized adults. Due to the lack of effect on fracture incidence and the increased incidence of nephrolithiasis in the intervention group of the WHI trial, the USPSTF concludes with moderate certainty that daily supplementation with 400 IU of vitamin D3 and 1000 mg of calcium has no net benefit for the primary prevention of fractures in noninstitutionalized, postmenopausal women. Although women enrolled in WHI were predominately white, the lower risk for fractures in nonwhite women makes it very unlikely that a benefit would exist in this population.
The final recommendations summarized as follows:
- insufficient evidence to determine benefit of calcium & vitamin D supplements in premenopausal women or in men to prevent fractures
- insufficient evidence to determine benefit of calcium (>1000 mg/day) and vitamin D (>400 IU/day) in postmenopausal women
- sufficient evidence to recommend against supplementation with calcium (<1000mg/day) and vitamin D (1000mg of calcium and >400IU of vitamin D) in postmenopausal women and older men.
It’s also nicely summarized in this handy table:
It also calls for prospective trials to study the benefits of vitamin D and calcium supplementation in early adulthood on fracture incidence later in life. Quite frankly, we’ll be waiting decades for this — if it ever appears.
Conclusion
Assuming benefit from a drug or supplement, in the absence of confirming evidence, can lead to bad health care decision-making. Yet we do this all the time, particularly with supplements that are generally believed to be safe and effective. These studies show that supplements can indeed be rigorously studied, and that surprising findings can emerge. Not only have calcium supplements been closely scrutinized for therapeutic use in dozens of prospective clinical trials, the evidence suggests that use in the absence of deficiency is at best, probably useless, and at worst, substantially elevating the risk of heart attacks and cardiovascular death. Without any clearly established benefits for most people, but exhibiting worrying signs of harms, it’s time to take the health halo off calcium supplements.
References
Li K., Kaaks R., Linseisen J. & Rohrmann S. (2012). Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the Heidelberg cohort of the European Prospective Investigation into Cancer and Nutrition study (EPIC-Heidelberg), Heart, 98 (12) 920-925. DOI: 10.1136/heartjnl-2011-301345
Xiao Q. Dietary and Supplemental Calcium Intake and Cardiovascular Disease Mortality: The National Institutes of Health–AARP Diet and Health StudyCalcium Intake and CVD Mortality, JAMA Internal Medicine, 1. DOI: 10.1001/jamainternmed.2013.3283
Moyer V. (2013). Vitamin D and Calcium Supplementation to Prevent Fractures in Adults: U.S. Preventive Services Task Force Recommendation Statement, Ann Intern Med, DOI: 10.7326/0003-4819-158-9-201305070-00603