Category: Medical Ethics
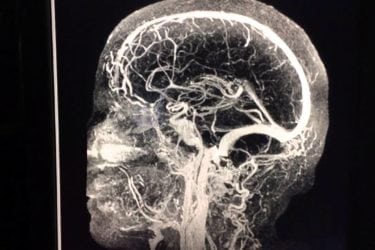
Clínica 0-19: False hope in Monterrey for brain cancer patients (part 3)
This is the conclusion of my series on Clínica 0-19, the cancer clinic where Drs. Alberto Siller and Alberto Garcia see patients with DIPG, a deadly brain tumor, whom they treat at Hospital Angeles in Monterrey Mexico with an unproven combination of intra-arterial chemotherapy with up to 11 drugs and a poorly defined dendritic cell immunotherapy. Some people have asked me: What's...

Right-to-try is now law. Let patients beware!
Last week, President Trump signed the worst federal right-to-try bill under consideration by Congress into law. Its purpose was never to help terminally ill patients, and now that it's law there will be nothing the FDA can do to protect vulnerable terminally ill patients who choose it. That's a feature, not a bug. That's because right-to-try is the result of a collaboration...
Doc Doc Zeus: A Glimpse Behind the Scenes of Medical Boards
A novel about a doctor who raped a minor and is being investigated by his state medical board provides behind-the-scene insights into the workings of medical boards. It helps explain why these boards are so often ineffective, why medical malfeasance so often leads to a token disciplinary action rather than to loss of license.
Corrigendum. The Week in Review for 05/21/2017
Choosing CAM leads to bad outcomes the world over. How deep can an acupuncture needle go? Measles continues and Minnesotans and will be welcomed in Texas. Rat rectal stimulation for Science. And more.
Corrigendum. The Week in Review for 04/02/2017
Death from vaccine-preventable infections. Homeopathy and acupuncture do not work. There is a difference between cost and worth. And more.
Stem Cells for Macular Degeneration: Meticulous Science vs. Unethical Carelessness
Rigorous scientists stabilized a patient’s macular degeneration with a cutting-edge stem cell treatment; less rigorous scientists misapplied stem cell science and left three women blind.

Chinese BioMedical Research: Sturgeon’s Law In Action
A Chinese government investigation has found that 80%, yes eighty percent, of Chinese biomedical research is fabricated. I bet that is an underestimate for Traditional Chinese Pseudo-Medicine.




