Category: Medical Ethics

Revealed by the FDA: The results of the most recent inspection of the Burzynski Clinic
The results of the latest FDA inspection of the Burzynski Clinic are in. They aren't pretty. Why is this cancer quack still allowed to do his bogus clinical trials?

The sad saga of an Amish girl with a curable cancer whose parents are refusing chemotherapy in favor of “natural healing”
In Ohio, an Amish girl named Sarah Hershberger is refusing chemotherapy for her leukemia, and her parents are supporting her. Akron Children's Hospital has instituted legal action to ensure that she receives life-saving treatment. As a motley crew of consisting of supporters of alternative medicine and anti-government libertarians are rallying to Sarah's cause. Will this girl receive the life-saving treatment she needs?
Integrative Medicine’s Collateral Damage
Integrative medicine combines the practice of medicine with alternative medicine. Proponents tend to take a paragraph or two to say this, but that is what remains when boiled down to its essence. By putting this more concise definition together with Tim Minchin’s often-quoted observation about alternative medicine, you get: integrative medicine is the practice of medicine combined with medicine that either has...
Answering Our Critics, Part 2 of 2: What’s the Harm?
Last week I posted a list of 30 rebuttals to many of the recurrent criticisms that are made by people who don’t like what we say on SBM. I thought #30 deserved its own post; this is it. At the end, I’ve added a few items to the original list. What’s the harm in people trying CAM? Science-based medicine has been criticized...
When urgency to cure beats research ethics, bad things happen
Editor’s note: Just for your edification, here’s a “bonus” post. True, you might have seen this recently elsewhere, but it’s so appropriate for SBM that I couldn’t resist sharing it with those of you who might not read the other source where this was published recently. 🙂 I’ve written a lot about Stanislaw Burzynski and what I consider to be his unethical...
The Overuse of Antibiotics for Viral Infections in Children
“For every complex problem there is an answer that is clear, simple, and wrong.” -H. L. Mencken As I sit in an apartment full of unpacked boxes and grumpy children, only a few days removed from driving 1,600 miles to a 3rd floor walk-up and a better life just outside of Boston, I find the task of writing a post somewhat daunting....
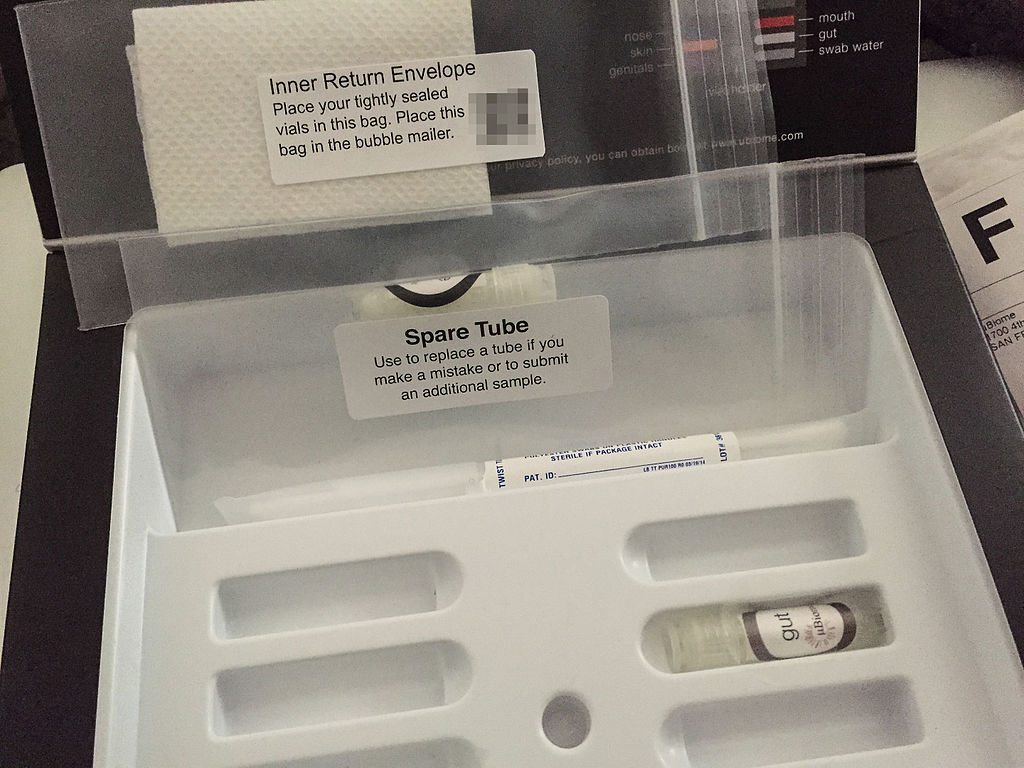
Meet Your Microbes: uBiome Offers New Service
We are not alone. Walt Whitman didn’t know how right he was when he said, “I contain multitudes.” The microbes on and in our bodies outnumber our own cells 10:1. Perhaps that creeps you out. Perhaps that makes you curious to know just who all these billions of creatures are that are using your body for a home and a transportation device....
Two Viewpoints
Most of what I read professionally is directed towards reality-based medicine. I spend my professional energies thinking about the application of reality to killing various and sundry microscopic pathogens. The conceptual framework I use, and that used by others in medicine, does not concern itself with the application of the Supplements, Complementary and Alternative Medicines that occupy the attention of this blog....
Angelina Jolie, radical strategies for cancer prevention, and genetics denialism
I had been debating whether to blog about Angelina Jolie’s announcement last week in a New York Times editorial entitled My Medical Choice that she had undergone bilateral prophylactic mastectomy because she had been discovered to have a mutation in the BRCA1 gene that is associated with a very high risk of breast cancer. On the one hand, it is my area...
Is thyroid replacement a performance-enhancing drug?
Has one physician uncovered the secret to Olympic Gold medals? And is that secret as simple as undiagnosed low thyroid function? That’s the question posed in a recent Wall Street Journal column entitled U.S. Track’s Unconventional Physician. Like the story that Steven Novella described yesterday, this narrative describes the medical practice of Dr. Jeffrey S. Brown, who sees thyroid illness where others...

