Mark Sircus and “natural allopathic medicine”? Now I’ve heard everything from quacks
The term "allopathic medicine" was invented by homeopaths in the 19th century as a disparaging term for medicine. So to see a quack like Mark Sircus try to coopt it as "natural allopathic medicine" is quite something.

Skeptics in the Pub. Cholera. Chapter 12b
I did not bother going back to the office but decided to wander over the sisters to see if they had anything new from their research. I took a trolley to Southeast and hopped off early. It was a beautiful summer day, and it would do me good to walk. It was a pretty neighborhood with many trees and well-kept gardens. I...

Some Doctors Cared Much More About Sore Arms Than Cold Bodies
The campaign against boosters was just a small part of a pathetic, pandemic-long pattern where doctors expressed grave concern about the mildest harms of measures to limit COVID, even purely theoretical ones, while being totally indifferent to literally anything the virus could do, including the deaths of children and young adults.

Measles Outbreaks on the Rise
The world is experiencing increasing outbreaks of a completely preventable disease. What's going wrong?

Best Hospital Eye Roll
Science: Figuring things out is better than making things up. A tee shirt I recently saw. Except… In a recent post Mayo Clinic Promotes Reiki, Steve seemed surprised that the Mayo was offering Reiki. I don’t know. Maybe he was channeling Louie. I know the Mayo is a top hospital, but I trained in Minneapolis at Hennepin County and we would have...

Denis Rancourt and “no virus”: COVID-19 symptoms were due psychological stress from the pandemic response!
It's hard to believe that in the 21st century there are still those who deny that viruses exist. However, virus denial and antivax go together and always have. Denis Rancourt, while far from the first or more vociferous virus denier, is an excellent example.

Dr. Jay Bhattacharya, April 2021: “The Central Problem Right Now I Think Is The Fear That People Still Feel About COVID.”
Doctors portrayed those who tried to avoid the virus as pathetic, disordered weaklings, afflicted by irrational panic, fear, and anxiety. It only makes sense if you remember one thing, they wanted you infected.

Skeptics in the Pub. Cholera. Chapter 12a
I slept like a rock, no dreams that I could remember, and upon awakening, the ball of anxiety that had been my constant companion was gone. I tried to get it back by thinking of all the unpleasant things that might happen in the next few days. Nothing. I felt good. Acceptance is the final stage of dying, so I must, at...

Some Good, But Preliminary Real World Data on Those Baby RSV Shots
The first post-rollout data for the RSV antibody shot looks pretty good, but far too many little ones missed out.
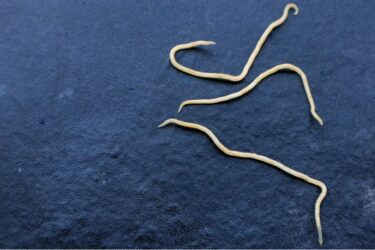
Parasite Cleanse
Tik Tok is a cesspool of wellness pseudoscience and misinformation. All of social media has the potential to spread misinformation without any filter, but for some reason Tik Tok has become the preferred platform for the most outrageous claims and nonsense. A recent trend on Tik Tok (and within the wellness community generally) is the parasite cleanse. The idea is that many...





