Tag: anecdote
The New York Times: Promoting False Hope as Journalism
The New York Times sells a narrative of false hope, and fails to engage in even basic journalism to tell a more complete story.
The Cancer Cure Anecdote
Dr. Ian Gawler, a veterinarian, suffered from osteogenic sarcoma (a form of bone cancer) of the right leg when he was 24 in 1975. Treatment of the cancer required amputation of the right leg. After completing treatment he was found to have lumps in his groin. His oncologist at the time was confident this was local spread from the original cancer, which...
When Further Research Is NOT Warranted: The “Wisdom of Crowds” Fallacy
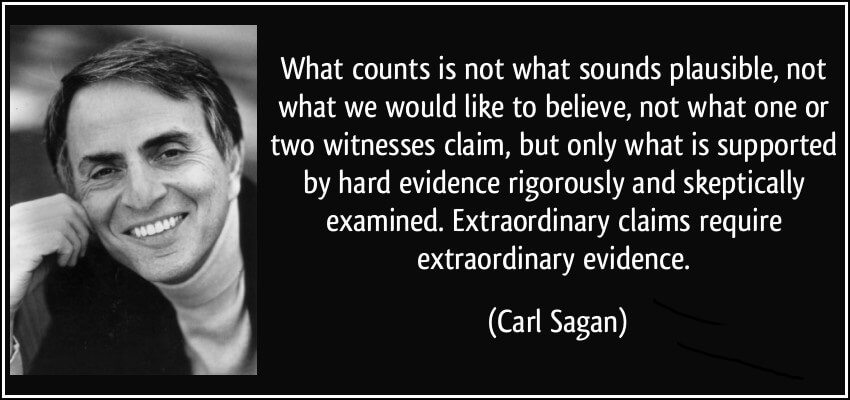
Most scientific research studies have at least one thing in common: the conclusion section ends with, “further research is warranted.” I’d say it’s about as common as the “talk to your doctor” disclaimer in TV ads for pharmaceutical products. And in a way, they both serve the same purpose. They’re a “CYA” move. What does “further research is warranted” mean in plain...


The “It Worked for Me” Gambit
It is almost inevitable that whenever we post an article critical of the claims being made for a particular treatment, alternative philosophy, or alternative profession, someone in the comments will counter a careful examination of published scientific evidence with an anecdote. Their arguments boils down to, “It worked for me, so all of your scientific evidence and plausibility is irrelevant.” Both components...