Tag: lung cancer
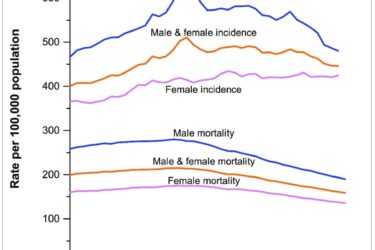
Cancer Death Rate Continues to Decline
The new data are in – cancer deaths continue to decline at a steady rate.

Alternative medicine kills cancer patients, “complementary” edition
By definition, alternative medicine has not been shown to be effective or has been shown to be ineffective. Thus, alternative medicine is ineffective against cancer and can best be represented as either no treatment at all or potentially harmful treatment. It is thus not surprising that cancer patients who choose alternative medicine have a higher risk of dying from their cancer. A...

Cancer, vitamin supplements, and unexpected consequences
Not only do B-vitamin supplements not protect you from lung cancer, they may significantly raise your risk of cancer.

CVS selling homeopathic remedies: It gets personal
I almost purchased a worthless homeopathic eye remedy at CVS for a cancer patient. I'm taking action to try to stop this from happening to others.

Diet and exercise versus cancer: A science-based view
Yes, diet and exercise can be useful to prevent some cancers. Unfortunately, they don't prevent all cancers, and the effect size is more modest than often represented. That's not to say that eating right and exercise aren't good. They are, for so many other reasons than cancer. Just don't view them as a panacea for preventing cancer.
“Liquid biopsies” for cancer screening: Life-saving tests, or overdiagnosis and overtreatment taken to a new level?
I’ve written many times about how the relationship between the early detection of cancer and decreased mortality from cancer is not nearly as straightforward as the average person—even the average doctor—thinks, the first time being in the very first year of this blog’s existence. Since then, the complexities and overpromising of various screening modalities designed to detect disease at an early, asymptomatic...
Recent Developments and Recurring Dilemmas in Cancer Screening: Colon, Lung, Thyroid
A new stool DNA test was recently approved by the FDA for colon cancer screening. My first reaction was “Yay! I hope it’s good enough to replace all those unpleasant, expensive screening colonoscopies.” But of course, things are never that simple. I wanted to explain the new test for our readers; but before I could start writing, some other issues in cancer...
Hyping Health Risks
Three kids on the same block were diagnosed with leukemia last year. That couldn’t happen just by chance, could it? There MUST be something in the environment that caused it (power lines, the chemical plant down the street, asbestos in their school, iPods, Twinkies?). Quick, let’s measure everything we can think of and compare exposures to other blocks and find an explanation....


