Tag: placebo
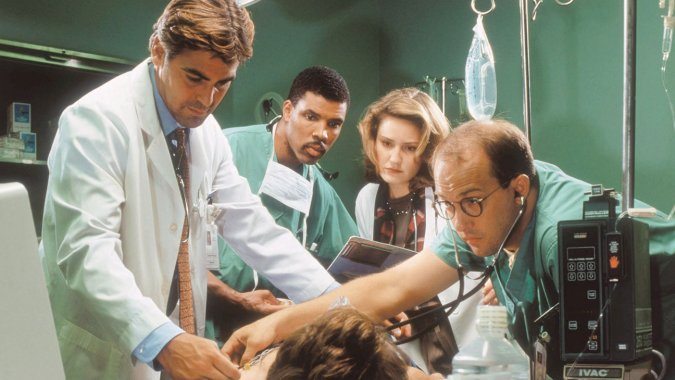
On the pointlessness of acupuncture in the emergency room…or anywhere else
As incredible as it seems, advocates of "integrative medicine" are on the verge of creating a new specialty, emergency acupuncture. I wish I were joking, but I'm not.
Curse Removal from the Annals. More Acupuncture Nonsense.
A short post this week. Last weekend was a busy call weekend and as I type this I am heading for Palm Springs for a long weekend of hiking in the desert. If there is no entry in 14 days, look for my bleached bones somewhere in Joshua Tree. Some observations about a recent article in the once-respected Annals of Internal Medicine,...
Is “harnessing the power of placebo” worthwhile to treat anything?
We frequently write about placebo effects here on Science-Based Medicine. The reason is simple. They are an important topic in medicine and, at least as importantly, understanding placebo effects is critical to understanding the exaggerated claims of advocates of “complementary and alternative medicine” (CAM), now more frequently called “integrative medicine” (i.e., integrating pseudoscience with science). Over the years, I (and, of course,...
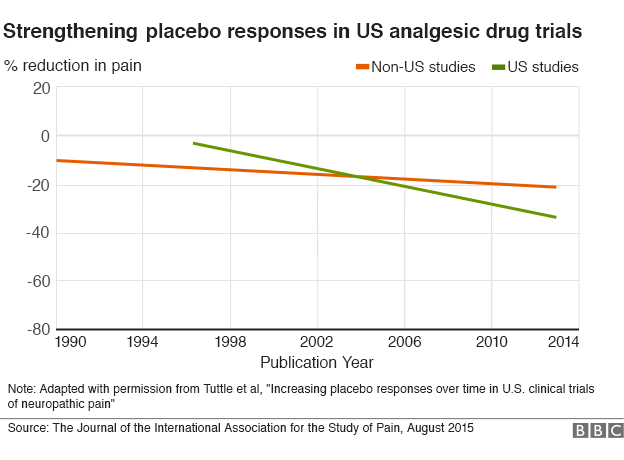
Are Placebos Getting Stronger?
A new study looked at clinical trials for neuropathic pain over the last 23 years and found that the response of subjects in the placebo group has been increasing over time, but only in the United States. The cause of this increase is unknown, and has provoked a fascinating discussion about the nature of placebos and their role in medical research. What...

The Worst Homeopathy Study. Ever
I run across a lot of information in my feeds that I need to save for further evaluation. The study “Does additional antimicrobial treatment have a better effect on URTI cough resolution than homeopathic symptomatic therapy alone? A real-life preliminary observational study in a pediatric population“, I saved with the file name, ‘jaw droppingly stupid’. The worst homeopathy clinical trial ever doesn’t...
Placebo by Conditioning
Truly understanding placebo effects (note the plural) is critical to science-based medicine. Misconceptions about placebo effects are perhaps the common problem I encounter among otherwise-scientific professionals and science communicators. The persistence of these misconceptions is due partly to the fact that false beliefs about placebos, namely that “the” placebo effect is mainly an expectation mind-over-matter effect, is deeply embedded in the culture....
Should placebos be used in randomized controlled trials of surgical interventions?
Trials of new experimental drugs frequently compare them to placebo, particularly when there is a large subjective component to the disease being treated, such as pain. In contrast, placebo-controlled trials are rarely undertaken in surgery, mainly because it's been considered ethically dicey to do sham surgery on one group. Should this change? Should we be more open to doing randomized, placebo-controlled surgery...
Mediocre Expectations: Acupuncture
I had a dickens of a time writing this entry. The last week has been spent in New York for NECSS. It is safe to say that New York has plenty of distractions for us Dug the Dog types. Reality may be a honey badger, but New York is a squirrel. I say that when I travel I usually do not come...
Placebo, Are You There?
By Jean Brissonnet, translation by Harriet Hall Note: This was originally published as “Placebo, es-tu là?” in Science et pseudo-sciences 294, p. 38-48. January 2011. It came to my attention in the course of an e-mail correspondence with the editors of that magazine, where one of my own articles was published in French translation in January 2015. I thought this was the...


The “It Worked for Me” Gambit
It is almost inevitable that whenever we post an article critical of the claims being made for a particular treatment, alternative philosophy, or alternative profession, someone in the comments will counter a careful examination of published scientific evidence with an anecdote. Their arguments boils down to, “It worked for me, so all of your scientific evidence and plausibility is irrelevant.” Both components...