Tag: science based medicine
Deconstructing Homeopathy Propaganda
The definition of “propaganda,” like so many things, is a bit fuzzy. The dictionary definition is: “information, especially of a biased or misleading nature, used to promote or publicize a particular political cause or point of view.” There is no sharp demarcation line, however. Speech occurs on a spectrum from obsessively objective, fair, balanced, and scholarly at one end, to deliberately deceptive...

Why Science-Based Medicine Matters
The regular contributors at Science-Based Medicine (SBM) work diligently every week to explore the world of science-based medicine and the gauzy, nebulous netherworld of fantasy-based medicine. They shine light on the leading edge of medical science, dissect the nuances of mainstream care, expose the misconceptions and sometimes the frank deceptions of so-called alternative medicine. Launching SBM on January 1, 2008, sbmadmin (Steven...

The hijacking of evidence-based medicine
A hero of the blog, John Ioannidis, worries that evidence-based medicine has been hijacked, and when Ioannidis says something we at SBM listen. But has EBM been "hijacked"?

What naturopaths say to each other when they think no one’s listening, part 2
It’s said that the true test of a person’s character is what he or she does and says when no one is watching. When it comes to science and medicine, naturopaths fail that test of character. Again. Antivaccine views and quackery? It's all there, with a dollop of paranoia.

On “integrative medicine” and walking and chewing gum at the same time
Evidence matters. Science matters. However, when advocates of "integrating" quackery into medicine via the vehicle of "integrative medicine" invoke weak science and poor quality evidence in conventional medicine in response to criticism, what they are really doing is deflecting attention away from their quackery. More importantly, advocates of science-based medicine are capable of walking and chewing gum at the same time. We...
Choosing Wisely: Changing medical practice is hard
One of the hardest things to do in medicine is to change practice in the face of scientific evidence that what you're doing isn't working. Quacks never change, but medicine does. The change might be slower and messier than we would like, but change does happen. Choosing Wisely is an initiative designed to bring about change by discouraging the use of interventions...
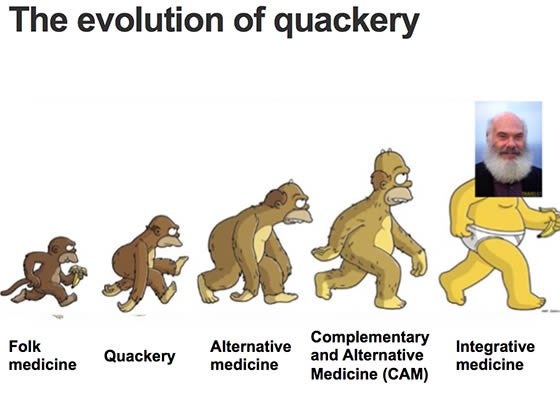
We Should Abandon the Concept of “Alternative Medicine”
In a recent editorial for the New York Times, Aaron E. Carroll argues, “Labels Like ‘Alternative Medicine’ Don’t Matter. The Science Does.” I agree with this headline thesis, but the details of his argument ironically show the harm that the so-called CAM (complementary and alternative medicine) movement has done. Carroll starts out well, essentially pointing out that the division between “conventional” and...
Remembering Wallace Sampson
I’m sad to report that Dr. Wallace (Wally) Sampson, one of the original authors at Science-Based Medicine, passed away on May 25th at the age of 85. Wally was a valued member of the SBM community, a mentor to many of us, and a tireless crusader against health fraud and pseudoscience in medicine. He carried the banner of defending science and reason...


Responding to SBM Critics
A response to a critic of SBM, and setting the record straight on our actual positions regarding evidence and the practice of medicine.