The President’s Council of Advisors on Science and Technology recently submitted its report to the President in which they stated that this influenza season might kill 30-90,000 people in the US. This forecast of the upcoming season caught the media’s attention and appears to have stoked the public interest in influenza. We have had many requests for more information about influenza here at SBM, and so in this post I am going to discuss the basics of influenza and try to put the current pandemic and upcoming season in perspective.
I find it is best to start at the beginning.
What Is influenza?
Within the public sphere, “The flu” has become shorthand for “I feel like crap.” I suspect that this is part of the reason why some people think the influenza vaccine doesn’t work. Medically speaking, however, influenza is a very specific family of viruses that cause a reasonably narrow set of problems for humans.
The influenza season in the Northern hemisphere usually runs from October through May, with a peak mid-February. Every season in the US between 5-20% of the US population is infected by influenza, and while the majority of people recover well from an influenza infection, not everyone will. Annually 200,000 people are hospitalized, and on average 36,000 will die either from influenza or its complications.
The classic influenza infection incubates for 1-4 days after exposure. Its onset is rapid, with most people experiencing high fever, headache, muscle aches, dry cough, sore throat, and nasal congestion. Gastro-intestinal symptoms like nausea, vomiting, and diarrhea are less common. Symptoms last from several days to almost two weeks, and a person is contagious from one day before symptoms begin to more than a week after symptom onset.
There are many strains of influenza. The current seasonal influenza is made up of three different influenza subtypes: A(H3N2), A(H1N1), and B. Don’t confuse the seasonal A(H1N1) strain with the current pandemic 2009 A(H1N1); they are distinct. I will refer to them as A(H1N1) for the seasonal strain, and 2009 (H1N1) for the pandemic “swine flu” strain. Influenza B is less common, less virulent, has a slower mutation rate, and is thus a lesser risk; the rest of this discussion is focused on Influenza A.
How does influenza spread?
Influenza has two dominant modes of transmission: droplet and contact transmission. Droplet means that when someone coughs or sneezes, extremely fine (and sometimes not-so-fine) droplets are aerosolized into the air around them. If these droplets come in contact with your nose, mouth, throat, or lungs, it is possible for you to become infected by the viruses in those droplets.
The second way influenza can be spread is either through direct contact or through an intermediate like a doorknob, known as a “fomite.” The virus can survive for minutes to days depending on the surface, and if you touch that surface then your mouth or nose, again, it is possible that you can become infected. Influenza does not appear to be capable of spreading long distances through the air (across large rooms or through air vents).
How does influenza change?
Influenza A is a versatile virus with many distinct serotypes. Most people are familiar with human, bird, and swine influenza, but influenza is in fact able to infect a large number of avian and mammalian species on the planet. It is important to realize that these viruses are not, despite their name, truly species specific. Random mutations and natural selection frequently create new strains of influenza capable of infecting other species; in its ability to mutate influenza is unparalleled.
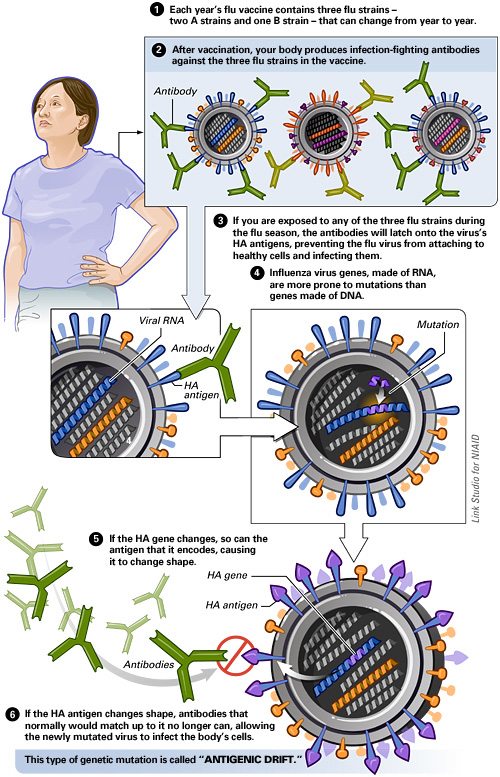
Influenza is an RNA virus encoded by just 11 genes on 8 separate RNA segments. With only 11 genes, you can see that influenza is a relatively simple virus. But its simplicity is one of the most significant reasons for its success. Unlike our DNA, the RNA of influenza replicates without the benefit of enzymes that correct transcription errors. This means that it makes more transcription errors, a lot more. One in every 1,000-10,000 nucleotides is mis-transcribed by influenza, giving it one of the highest mutation rates known. Some of these errors are neutral and have no effect on the virus. Some are detrimental and will result in a defective virus. But some of them are beneficial. Two genes encode influenza’s characteristic surface proteins hemagglutinin (HA) and neuraminidase (NA). There are 16 types of HA, 9 of NA, and respectively these two proteins serve to bind the virus to a target cell and to release new viral particles from a host cell, and they also happen to be the parts of influenza the immune system recognizes. Every so often a transcription error will change the conformation of either HA or NA just enough so that it cannot be recognized by the immune system. Voilà, we have a new strain of influenza, and your immune system has to start from scratch. This is the concept of “antigenic drift,” and it is responsible for the variation in influenza strains we see every year.
But that is only part of the story. Do you remember the 8 separate RNA segments? If a cell is infected with a single strain of influenza this is an inconsequential factoid. However, if two dissimilar strains of influenza co-infect the same cell, those 8 RNA segments become exceedingly important. Up to 256 unique combinations can result from that one pairing. Instead of a slow drift in the surface markers of the circulating influenza strains, suddenly we have a major re-assortment, and a brand-new strain is created. This is “antigenic shift,” and this is how the 2009 (H1N1) strain was born.
I hope it is clear at this point that influenza is not a single virus that changes over time, but is instead a family of viruses that to a greater or lesser extent co-exist and are constantly changing. Were it stable, your immune system would be able to establish meaningful immunity. Until we discover a way to make your immune system target a stable section of influenza, our best hope is to constantly redesign our vaccines against a moving target.
What makes the novel influenza A 2009 (H1N1) so special?
Other novel influenzas have been identified in the past without causing a pandemic. The 1976 swine flu is a prime example. Identified in Fort Dix, it infected at least 13 soldiers, killing one. It looked similar to the 1918 Spanish flu, which raised concerns of a potential pandemic and triggered a mass vaccination campaign. Yet it never spread beyond the base and has not been seen since.
Another example is the H5N1 “bird flu” that we’ve heard about since its emergence in 1997. It has had several outbreaks, caused over 167 deaths, and carries a ~60% mortality rate for those infected. Fortunately, though it can spread like wildfire through birds, and humans can catch it from birds, humans cannot reliably spread it to other humans. Thus it is a virus with the potential to be truly terrifying, but in its current state poses a limited infectious risk.
Why then are we so confident that the 2009 (H1N1) strain will behave differently and pose a real risk? Three reasons:
- First, recall that the 2009 (H1N1) is distinct from the seasonal A (H1N1). It appears to be a “triple recombination,” with characteristics derived from human, bird, and swine influenzas. When our population was tested for antibodies against 2009 (H1N1) nearly no children, and less than 10% of those under the age of 65 had reactive antibodies, and of those over 65 only 33% showed any response. It seems no one has seen a similar influenza in half a century. This means that the vast majority of our population is susceptible to infection this season; you can see the potential for infection on a grand scale.
- Second, unlike the 1976 strain, the 2009 (H1N1) has already proven itself to be highly contagious. From its first appearance in Mexico on March 18th, 2009, it took 4 weeks to spread outside the borders of Mexico, and within 2 more weeks it was in 5 states and 8 other nations. Only 6 weeks after being first identified, over 3,000 cases were to be found in 43 states and 23 countries, and on June 11th, 2009, after only 3 months, it had achieved pandemic status. Furthermore, it was able to accomplish all this during the season least conducive to its normal spread.
- Finally, the 2009 (H1N1) has proven itself to be far from benign. As of August 22nd, the US has hospitalized 8,843 people with 2009 (H1N1), and 556 have died, 101 of them under the age of 24. We have a hospitalization rate of 4.5/100,000 for ages 0-4, and 2.1/100,000 for ages 5-24. All of this, recall, has happened during influenza’s off-season.
In areas where 2009 (H1N1) emerged during the traditional influenza season, like Australia, they have reported more than a doubling in the number of people hospitalized from influenza, with around 1 in 5 requiring ICU-level care. Similar to what we have seen in the US, Australia has likewise demonstrated that 2009 (H1N1) has a higher attack rate in younger people, which is in stark contrast to the normal seasonal influenza pattern, and has shifted its mean age of death from influenza from 83 down to 54. Unlike what we have seen thus far, Australia has had a much higher hospitalization rate of 34.6/100,000 in ages 0-4, and an overall rate of 12/100,000 for the population. This likely reflects the differences between being on-season and off-season.
That is what makes 2009 (H1N1) so concerning. It is capable of causing serious infections even and perhaps especially in the young and the healthy. It is highly contagious, it has a worldwide population without immunity, and it now exists in low levels in most communities around the nation. And we are now entering into its prime season.
Conclusion: It’s the end of the world as we know it?
So is this the Zombie Apocalypse, or only slightly less concerning, is this going to be a repeat of the 1918 Spanish influenza pandemic? Almost certainly not. Nor, however, were the predictions made by the President’s Council of Advisors on Science and Technology outlandish fear mongering. 30,000 dead is an average influenza season, and if we see a simple doubling in the number of cases we will rapidly approach the higher end of their estimate.
Influenza warrants our respect and attention. I hope these estimates are higher than what we will in reality see; it would make my winter in the ICU far more pleasant. The fact remains that only time will tell. In the meantime, we would be wise to be prepared.
So what can you do?
- Get vaccinated against seasonal flu and 2009 (H1N1) – It’s cheap, safe, and effective. If you don’t get sick, you avoid all of the risks of infection while also avoiding the responsibility of infecting others.
- Wash your hands – You should be doing this anyway.
- Cover your cough and sneeze – It’s just polite not to spray your mucous in my face. Thank you.
- If you are ill stay home until 24 hours after your fever abates – If you are infected, there is no reason to risk the health of everyone around you.
- Don’t Panic – Most people will get through an influenza infection without medical attention. Rest, stay hydrated, and minimize your exposure to others.
The CDC recommendations for warning signs to seek medical care are as follows:
In children, emergency warning signs that need urgent medical attention include:
- Fast breathing or trouble breathing
- Bluish or gray skin color
- Not drinking enough fluids
- Severe or persistent vomiting
- Not waking up or not interacting
- Being so irritable that the child does not want to be held
- Flu-like symptoms improve but then return with fever and worse cough
- Any child under 12 weeks of age with fever over 100.4 F (38 C)
In adults, emergency warning signs that need urgent medical attention include:
- Difficulty breathing or shortness of breath
- Pain or pressure in the chest or abdomen
- Sudden dizziness
- Confusion
- Severe or persistent vomiting
- Flu-like symptoms improve but then return with fever and worse cough
