Medicare and Medicaid place restrictions on new Alzheimer’s drug, Aduhelm (aducanumab)
An important decision has been made about a controversial new drug to treat Alzheimer's disease.

Detox: What “They” Don’t Want You To Know
Before you start your New Year’s detox, here's a tip that will save you time, money, and possibly your health.
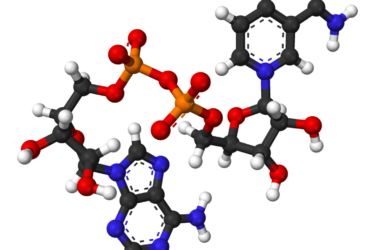
NAD Therapy
NAD therapy is touted as a cure-all for addiction and several chronic diseases. Evidence supporting these claims is lacking.

Pandemic drives huge surge in herbal remedy sales
The COVID-19 pandemic has fueled a boom in herbal supplement sales.
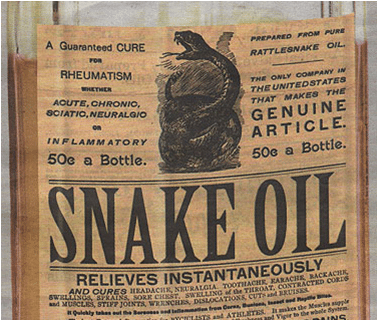
Long COVID: Alternative medicine sees a business opportunity
With vaccines transforming the risk and consequences of a COVID infection, the health burden of "long COVID" may become a lasting consequence of the pandemic. Alternative medicine senses a business opportunity.

Closing the vaccine hesitancy gap
What tactics and strategies should be used to address COVID-19 vaccine hesitancy?

The risks associated with alternative medicine
In a new paper, the types and severity of harms from different types of alternative medicine are described.

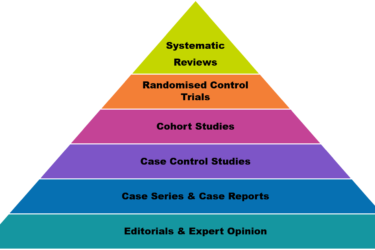
No evidence, no problem: A closer look at the aducanumab approval
Why did the FDA approve aducanumab, a drug that hasn't been shown to work?

Can GMOs cause gastrointestinal sensitivity and inflammation?
A closer look at the widespread claim that GMOs cause bowel irritation and inflammation.